- Main Page
- A1C Test
- Advance Directives
- Age on other Planets
- Aliens
- American Flag
- Annuals
- Anxiety
- Aortic Aneurysm
- Apple Cider Vinegar
- Arrhythmia
- Atrial Fibrillation
- Avoiding Scams
- Awareness Ribbons
- Bamboo
- Banana Tree, Grand Nain
- Banana Tree, Ice Cream
- Banana Tree, Zebrina Rojo
- Beekeeping
- Benign P P Vertigo
- Birth Month
- Blood Tests
- Blood Types
- Body Mass Index - BMI
- BMI Calculator
- Boogaloo
- Bookmarks
- Boot Anatomy
- Boot Fit Guide
- Boot Glossary
- Boot Leathers
- Boot Makers
- Boot Retailers
- Boot Styles - Western
- Boot Toes & Heels - Western
- Boot Toes & Heels - Work
- Bronchitis
- Candle Colors
- Carbohydrates
- Cardiac Catheterization
- Cardiovascular Disease
- CGM's
- Chakras
- Chinese Zodiac
- Cholesterol
- Christmas Tree
- Color Codes Chart
- C.O.P.D.
- Coronary Artery Disease
- Country Stars
- Cowboy Hat Etiquette
- Cowboy Hat Sizing
- C.P.A.P.
- Credit Score Checkers
- Crystals & Gems
- CT scan
- Degenerative Disk Disease
- Depression
- Diabetes Info.
- Diabetes Facts
- Diabetes - Pre
- Diabetes - Type 1
- Diabetes - Type 2
- Diabetes - Type 3c
- Diabetes - Gestational
- Diabetes Care
- Diabetes Care Team
- Diabetes Terms
- Diabetes Treatment
- Diabetes & Fruits
- Diabetes & Veg's
- Diet - Boiled Egg
- Diet - DASH
- Diet - Fat Burning
- Diet - Mediterranean
- Diet - Military
- Disability
- Do Not Resuscitate
- Dream Catchers
- Dupixent®
- Echocardiogram
- Electrocardiogram
- Emphysema
- Epsom Salt
- Eye Teasers
- Fairies
- Farxiga®
- Flower Astrology
- Fonts
- Foods To Regrow
- Friend
- Funny Things
- Fun Stuff
- Glycemic Index
- Gout
- Growing Blueberries
- Halloween
- Halloween Treats
- Headaches
- Health Info. Lines
- Heart Attack
- Heart Disease - Other
- Heart Failure
- Heart Tests
- Hello!!
- Herbal Codes
- Herbal Medicine
- Herb & Oils Uses
- Herniated disk
- Home Remedies
- House Plants
- Humalog®
- Hydrogen Peroxide
- Hyperglycemia
- Hypoglycemia
- Hyperkalemia
- Hypokalemia
- Hypertension
- Hypotension
- Important Numbers
- Insomnia
- Insulin
- Juice Recipes
- Karma
- Kidney Cysts
- Kidney Disease
- Kinds of Tea
- Lantus®
- Lemon Cleanse
- Logger vs Lineman
- Macaroni!!
- Medicare
- Mental Health
- MO HealthNet
- Moon Phases
- Mounjaro®
- MRI Scan
- My Athletic Shoes
- My Boots & Spurs
- My Cowboy Hats
- Myelography
- Mystical Unicorn
- Nasal Polyps
- Natal Astrology Chart
- Never Forget
- Nuclear Medicine
- Nutrition - Adults
- Nutrition - Adults, Older
- Nutrition - Kids
- Obesity
- One Little Rose
- Orchid Growing
- Orchid Sources
- Pagan Humor
- Pagans vs.Wiccans
- Parking Spaces
- PayPal.Me
- Pentagram vs. Pentacle
- Perennials
- Peripheral Artery Disease
- PET/CT Scan
- PET Scan
- Phobias A-Z
- Plant Care
- Plant Zone Map
- Potassium
- Propagating Plants
- Prurigo Nodularis
- Psychic Gifts
- PVC's
- Quit Smoking
- Recipes I like
- Red Yeast Rice
- Roses
- Runes
- Sadie & Beethoven
- Salt & Sodium
- Salt Water Flush
- Sciatica
- Service Animals
- Shape Shifters
- Sleep Apnea
- Sleep Disorders
- Sleep Studies
- Smile
- SPECT Scan
- Speed Test
- Spices You Need
- Spices I Have
- Spinal Stenosis
- Stents
- Steel Toe vs. Comp. Toe
- Stress Test - Exercise
- Stress Test - Nuclear
- Sugars - Sweeteners
- Superstitions
- Symbols
- Tarot
- The Ten Commandments
- Tools of the Craft
- Top Expensive Movies
- Top Modern Westerns
- Top 100 Westerns
- Toyota Yaris 2008
- Toyota Yaris 2012
- Trazodone
- Tree, Calamondin Orange
- Tree, Lemon (Meyer)
- Tree, Lime
- Tree Signs
- Ultrasound
- US Bill of Rights
- US Constitution
- US Declaration of Independence
- Vaccines by Age
- Vaccines 0-6 yrs
- Vaccines 7-18 yrs
- Vaccines 19 and up
- Ventricular Fibrillation
- Vertigo
- Vital Records
- Vital Signs
- Vitamin B12
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin K
- Vitamins & Minerals
- Water Therapy
- Weight on other Planets
- Wiccan Rede
- X-Rays
- Yin / Yang
- Zodiac Signs
Needed to read PDF's
Sciatica
Overview
Sciatica is nerve pain from an injury or irritation to your sciatic nerve. In addition to pain, it can involve tingling or numbness in your back or butt that may also radiate down your leg. More severe symptoms are also possible.
Your sciatic nerve is the longest and thickest nerve in your body. It’s up to 2 centimeters wide (a U.S. penny or a United Kingdom 1 pence coin are about the same width). Despite its name, it’s not just one nerve. It’s actually a bundle of nerves that come from five nerve roots branching off from your spinal cord.
You have two sciatic nerves, one on each side of your body. Each sciatic nerve runs through your hip and buttock on one side. They each go down the leg on their side of your body until they reach just below your knee. Once there, they split into other nerves that connect to parts farther down, including your lower leg, foot and toes.
Having sciatica means you can experience mild to severe pain anywhere with nerves that connect to the sciatic nerve. The symptoms can affect your lower back, hips, buttocks or legs. Some symptoms may extend as far down as your feet and toes, depending on the specific nerve(s) affected.
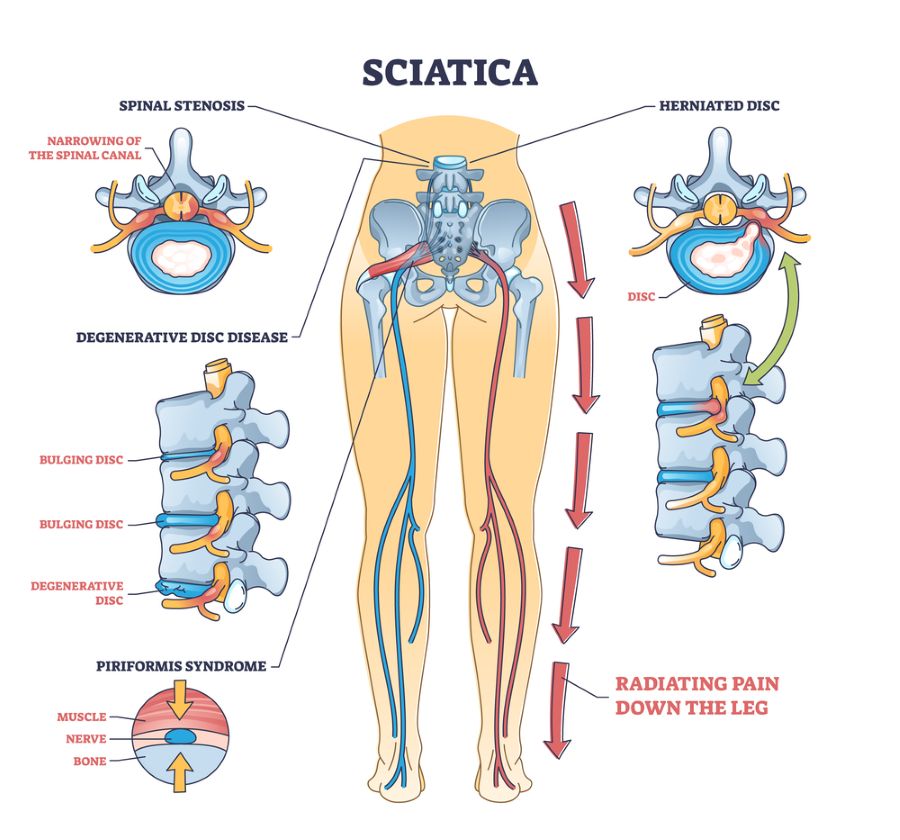
Click on picture for a full screen view
Types of sciatica
There are two types of sciatica. Regardless of what type you have, the effects are the same. The types are:
- True sciatica. This is any condition or injury that directly affects your sciatic nerve.
- Sciatica-like conditions. These are conditions that feel like sciatica, but happen for other reasons related to the sciatic nerve or the nerves that bundle together to form it.
Healthcare providers tend to refer to both types as just “sciatica.” The differences between them usually only matter when your healthcare provider determines how to treat it.
How common is sciatica?
Sciatica is a very common condition. About 40% of people in the U.S. experience some form of sciatica during their lifetime. It rarely happens before age 20 unless it’s injury-related.
Symptoms
Sciatica pain can be almost anywhere along the nerve pathway. It's especially likely to follow a path from the low back to the buttock and the back of a thigh and calf.
The pain can vary from a mild ache to a sharp, burning pain. Sometimes it feels like a jolt or electric shock. It can be worse when coughing or sneezing or sitting a long time. Usually, sciatica affects only one side of the body.
Some people also have numbness, tingling, or muscle weakness in the leg or foot. One part of the leg can be in pain, while another part can feel numb.
When to see a doctor
Mild sciatica usually goes away over time. Call your primary care professional if self-care measures don't ease symptoms. Also call if pain lasts longer than a week, is severe or gets worse.
Get immediate medical care for:
- Pain. Sciatica pain happens because of pressure on the affected nerve(s). Most people describe sciatica pain as burning or like an electric shock. This pain also often shoots or radiates down the leg on the affected side. Pain commonly happens with coughing, sneezing, bending or lifting your legs upward when lying on your back.
- Tingling or “pins and needles” (paresthesia). This is similar to the feeling you have when a leg falls asleep because you sat cross-legged.
- Numbness. This is when you can’t feel sensations on the skin in the affected areas of your back or leg. It happens because signals from your back or leg are having trouble reaching your brain.
- Muscle weakness. This is a more severe symptom. It means that muscle command signals are having trouble reaching their destinations in your back or legs.
- Urinary incontinence or fecal incontinence. This is a very severe symptom. It means signals that control your bladder and bowels aren’t reaching their destinations.
Causes
Sciatica can happen because of any condition that affects the sciatic nerve. It can also happen because of conditions affecting any of the five spinal nerves that bundle to form the sciatic nerve.
Conditions that can cause sciatica include:
- Herniated disks.
- Degenerative disk disease.
- Spinal stenosis.
- Foraminal stenosis.
- Spondylolisthesis.
- Osteoarthritis.
- Injuries.
- Pregnancy.
- Tumors, cysts or other growths.
- Conus medullas syndrome.
- Cauda equina syndrome.
Risk factors
Risk factors for sciatica include:
- Age. People ages 20 to 50 are most likely to have herniated disks. Bone spurs develop more commonly as people age.
- Obesity. Being overweight increases stress on the spine.
- Occupation. A job that requires twisting the back, carrying heavy loads or driving a motor vehicle for long periods might play a role in herniated disks.
- Prolonged sitting. People who sit a lot or don't move much are more likely to develop herniated disks than active people are.
- Diabetes. This condition, which affects the way the body uses blood sugar, increases the risk of nerve damage.
Complications
Most people recover fully from sciatica. However, a possible complication of sciatica is chronic (long-term) pain.
If there’s serious damage to an affected nerve, chronic muscle weakness, such as a “drop foot,” might happen. That’s when nerve damage causes numbness in your foot, which makes normal walking difficult or even impossible.
Sciatica can also potentially cause permanent nerve damage, resulting in a loss of feeling in the affected legs.Seek immediate medical attention for:
- Loss of feeling in the affected leg.
- Weakness in the affected leg.
- Loss of bowel or bladder control.
Prevention
Some causes of sciatica are preventable, but others happen unpredictably or for unknown reasons. For the causes that aren’t preventable, it may still be possible to reduce your risk of developing them
To protect your back:
- Exercise regularly. To keep the back strong, work the core muscles — the muscles in the abdomen and lower back needed for good posture and alignment. Physical activity can include everything from stretching to strength training. Increasing core strength and flexibility can improve back pain. Other forms of activity, such as aerobic exercise, can also help you reach and maintain a weight that’s healthy for you. A healthcare professional can recommend activities.
- Keep good posture when sitting. Choose a seat with good lower back support, armrests and a swivel base. For better low back support, place a pillow or rolled towel in the small of the back to keep its normal curve. Keep knees and hips level.
- Use your body correctly. When standing for long periods, rest one foot on a stool or small box from time to time. When lifting something heavy, let your legs do the work. Hold the load close to your body. Don't lift and twist at the same time. Find someone to help lift heavy or awkward things.
- Quit (or don’t start) using tobacco products. Nicotine from any source (including vaping) reduces blood supply to your bones, which can weaken your spine and its various components.
- Reach and maintain a weight that’s healthy for you. Your primary care provider can guide you on how to eat and get physical activity. Make sure you get enough calcium and vitamin D for bone health, too.
- Protect yourself from falls. Wear shoes that fit and keep stairs and walkways free of clutter to reduce your chance of a fall. Make sure rooms are well-lit, and there are grab bars in bathrooms and rails on stairways.
- Take time to recover if needed. Don’t try to work through back pain. That can lead to even worse injuries. Back pain doesn’t have to keep you from being active, either. You can still participate in low-impact activities such as swimming, walking, yoga or tai chi.
.
Diagnosis
A healthcare provider can diagnose sciatica using a combination of methods. They’ll review your medical history and ask about your symptoms. They’ll also do a physical examination. That exam will include:
- Walking. Sciatica often causes visible changes in how you walk. Your provider will watch for those changes as part of diagnosing sciatica.
- Straight leg raise test. This involves having you lie on an exam table with your legs straight out. They’ll slowly raise your legs one at a time toward the ceiling and ask when you start to feel pain or other symptoms. These can help pinpoint the cause of sciatica and how to manage it.
- Other flexibility and strength checks. These can help your provider determine if any other factors are causing or contributing to your sciatica.
Tests
People with severe pain or pain that doesn't improve within a few weeks may need:
- X-ray. A spine X-ray is an imaging test that uses electromagnetic waves to take detailed pictures of the bones in your neck and back. You might need spinal X-rays if you were born with structural spine issues or if you have pain from trauma or conditions like arthritis or osteoporosis.
- MRI. An MRI (magnetic resonance imaging) scan is a test that creates clear images of the structures inside your body using a large magnet, radio waves and a computer. Healthcare providers use MRIs to evaluate, diagnose and monitor several different medical conditions.
- CT scan. A CT (computed tomography) scan is an imaging test that helps healthcare providers detect diseases and injuries. It uses a series of X-rays and a computer to create detailed images of your bones and soft tissues. A CT scan is painless and noninvasive. You might go to a hospital or imaging center for your CT scan.
- Nerve conduction velocity studies. A nerve conduction study is a test that can help diagnose issues with your peripheral nerves, such as peripheral neuropathy and nerve compression syndromes. Healthcare providers often use this test alongside an EMG (electromyography) test.
- Electromyography (EMG). Neurologists use electromyography (EMG) to help diagnose injuries and conditions that affect your muscles and the nerves that control them, such as carpal tunnel syndrome and muscular dystrophy. They often use this test alongside a nerve conduction study.
- Myelogram. A myelogram is an imaging test that uses a contrast material and X-rays or computed tomography (CT) scans to get detailed pictures of your spine. Healthcare providers might recommend a myelogram if you have chronic back pain.
Treatment
For pain that doesn't improve with self-care measures, some of the following treatments might help.
Medications
The types of medicines that might be used to treat sciatica pain include:
- Anti-inflammatories.
- Corticosteroids.
- Antidepressants.
- Anti-seizure medications.
- Opioids.
Physical therapy
Once the pain improves, a healthcare professional can design a program to help prevent future injuries. This typically includes exercises to correct posture, strengthen the core and improve range of motion. The goal of physical therapy is to find exercise movements that decrease sciatica by reducing pressure on the nerve. Options include stretching exercises or low-impact activities like walking, swimming or water aerobics.
Steroid injections
Injections like corticosteroids may provide short-term relief (typically up to three months). These usually involve local anesthesia, so there’s less discomfort. Your healthcare provider can tell you more about this process.
Surgery
Surgery may be the best option when sciatica is more severe. Usually, healthcare providers don’t recommend surgery unless you have symptoms that indicate nerve damage is happening or imminent. They may also recommend surgery if you have severe pain that prevents you from working or going about your usual routine, or if your symptoms don’t improve after six to eight weeks of conservative treatment.
Surgery options to relieve sciatica include:
- Diskectomy. This is a surgery that removes fragments or small sections of a herniated disk that are pressing on a nerve.
- Laminectomy. Each vertebra has a rear section called the lamina (it’s on the side of the vertebra just underneath the skin of your back). A laminectomy involves removing a section of the lamina that’s pressing on spinal nerves.
Lifestyle and home remedies
For most people, sciatica responds to self-care measures. Although resting for a day or so may provide relief, staying inactive will make symptoms worse.
Other self-care treatments that might help include:
- Cold packs. Place a cold pack on the painful area for up to 20 minutes several times a day. Use an ice pack or a package of frozen peas wrapped in a clean towel.
- Hot packs. After 2 to 3 days, apply heat to the areas that hurt. Use hot packs, a heat lamp or a heating pad on the lowest setting. For continuing pain, try using both warm and cold packs, one at a time.
- Stretching. Stretching exercises for the low back might provide some relief. Try to hold the stretch for at least 30 seconds. Avoid jerking, bouncing or twisting during the stretch.
- Medications. Pain relievers such as ibuprofen (Advil, Motrin IB, others) and naproxen sodium (Aleve) are sometimes helpful for sciatica. Use only as directed.
Alternative medicine
Alternative therapies often used for low back pain include:
- Acupuncture. The acupuncturist inserts hair-thin needles into the skin at certain points on the body. Some studies have suggested that acupuncture can help back pain, while others have found no benefit. If you decide to try acupuncture, choose a licensed professional.
- Chiropractic. Chiropractors can make spinal adjustments or manipulations to restore spinal movement and decrease pain. Spinal manipulation appears to work and to be as safe as standard treatments for low back pain.
- Massage therapy. Massages can help loosen up the larger muscles in the back and hips that may be tight or have spasms.
Preparing for your appointment
Not everyone who has sciatica needs medical care. If your symptoms are serious or last for more than a month, make an appointment with your healthcare professional.
What you can do
- Write down your symptoms and when they began.
- List key medical information, including other conditions you have and the names and doses of medications, vitamins or supplements you take.
- Note recent accidents or injuries that might have damaged your back.
- Take a family member or friend along, if possible. Someone who accompanies you can help you remember the information you get.
- Write down questions to ask your healthcare professional.
For radiating low back pain, some basic questions to ask include:
- What's the most likely cause of my back pain?
- Are there other possible causes?
- What tests do I need?
- What treatment do you recommend?
- Should I have surgery? Why or why not?
- Are there restrictions I need to follow?
- What self-care measures should I take?
- What can I do to keep my symptoms from coming back?
Don't hesitate to ask other questions.
What to expect from your doctor
Your doctor is likely to ask you a number of questions, such as:
- Do you have numbness or weakness in your legs?
- Do some body positions or activities make your pain better or worse?
- How much does your pain limit your activities?
- Do you do heavy physical work?
- Do you exercise regularly? If yes, with what types of activities?
- What treatments or self-care measures have you tried? Has anything helped?
When should I go to the emergency room?
You should get emergency medical attention if you experience the following:
- Any muscle weakness.
- Loss of bowel or bladder control.
- Severe pain that keeps you from your usual activities and lasts for more than a few hours.
- Sudden severe pain, numbness or any other sciatica symptoms immediately after a fall, car crash or any other injury-causing event.
Additional Common Questions
Can sciatica occur down both legs?
Sciatica usually affects only one leg at a time. However, sciatica can occur in both legs in rare cases.
Does sciatica occur suddenly, or does it take time to develop?
Sciatica can come on suddenly or gradually. It depends on the cause. A disk herniation or injury can cause sudden pain. Arthritis in your spine or other degenerative conditions develop slowly over time.
Can weight gain during pregnancy cause sciatica?
Sciatica is common in pregnancy but isn’t usually related to pregnancy weight changes. Two main factors better explain why it’s more likely to happen during pregnancy.
The first explanation has to do with pregnancy-related hormones. Those hormones can cause a loosening of ligaments and connective tissue in your spine. That loosening makes your spine more flexible, which can cause disk slippage, pinched nerves and sciatica.
The weight and position of the fetus can also press on the nerve.
The good news is there are ways to ease sciatic pain during pregnancy, and the pain should go away after birth. Physical therapy and massage therapy, warm showers, heat, medications and other measures can help. Practicing good posture techniques during pregnancy can also help.
How can I tell if pain in my hip is a hip issue or sciatica?
Hip problems, such as arthritis in your hip, usually cause pain in your groin, or pain when you put weight on your leg or move it around.
If your pain starts in your back and moves or radiates toward your hip or down your leg, or you have numbness, tingling or weakness, sciatica is the most likely cause.
Sciatica vs. radiculopathy — what’s the difference?
Radiculopathy is a broader term that describes the symptoms caused by a pinched nerve in your spine. Sciatica is the most common type of radiculopathy.
Should I rest if I have sciatica?
Rest is helpful during the first two days you have sciatica. But total rest isn’t likely to help, and physical inactivity can make your pain worse and slow healing. The goal is to find a balance so you’re active enough to stay flexible and maintain strength but not make sciatica worse or injure yourself. A healthcare provider can guide you on how to find this balance and help you recover.
Can sciatica cause my leg and/or ankle to swell?
Sciatica from a herniated disk, spinal stenosis or bone spurs can cause inflammation or swelling in the affected leg. Piriformis syndrome complications can also cause leg swelling.
One Final Note..
Sciatica pain in your back, butt or legs can disrupt your life in many ways. Fortunately, there’s a lot you can do to help yourself recover. You can often treat milder cases yourself. More intense symptoms are also often treatable. Surgery usually isn’t necessary, but it’s an option if your symptoms are severe. With treatment, you can put sciatica behind you and return to living on your terms.
Find me on Social Media
 |
Don't forget to bookmark me to see updates.. Copyright © 2000 - 2025 K.
Kerr |







