- Main Page
- A1C Test
- Advance Directives
- Age on other Planets
- Aliens
- American Flag
- Annuals
- Anxiety
- Aortic Aneurysm
- Apple Cider Vinegar
- Arrhythmia
- Atrial Fibrillation
- Avoiding Scams
- Awareness Ribbons
- Bamboo
- Banana Tree, Grand Nain
- Banana Tree, Ice Cream
- Banana Tree, Zebrina Rojo
- Beekeeping
- Benign P P Vertigo
- Birth Month
- Blood Tests
- Blood Types
- Body Mass Index - BMI
- BMI Calculator
- Boogaloo
- Bookmarks
- Boot Anatomy
- Boot Fit Guide
- Boot Glossary
- Boot Leathers
- Boot Makers
- Boot Retailers
- Boot Styles - Western
- Boot Toes & Heels - Western
- Boot Toes & Heels - Work
- Bronchitis
- Candle Colors
- Carbohydrates
- Cardiac Catheterization
- Cardiovascular Disease
- CGM's
- Chakras
- Chinese Zodiac
- Cholesterol
- Christmas Tree
- Color Codes Chart
- C.O.P.D.
- Coronary Artery Disease
- Country Stars
- Cowboy Hat Etiquette
- Cowboy Hat Sizing
- C.P.A.P.
- Credit Score Checkers
- Crystals & Gems
- CT scan
- Degenerative Disk Disease
- Depression
- Diabetes Info.
- Diabetes Facts
- Diabetes - Pre
- Diabetes - Type 1
- Diabetes - Type 2
- Diabetes - Type 3c
- Diabetes - Gestational
- Diabetes Care
- Diabetes Care Team
- Diabetes Terms
- Diabetes Treatment
- Diabetes & Fruits
- Diabetes & Veg's
- Diet - Boiled Egg
- Diet - DASH
- Diet - Fat Burning
- Diet - Mediterranean
- Diet - Military
- Disability
- Do Not Resuscitate
- Dream Catchers
- Dupixent®
- Echocardiogram
- Electrocardiogram
- Emphysema
- Epsom Salt
- Eye Teasers
- Fairies
- Farxiga®
- Flower Astrology
- Fonts
- Foods To Regrow
- Friend
- Funny Things
- Fun Stuff
- Glycemic Index
- Gout
- Growing Blueberries
- Halloween
- Halloween Treats
- Headaches
- Health Info. Lines
- Heart Attack
- Heart Disease - Other
- Heart Failure
- Heart Tests
- Hello!!
- Herbal Codes
- Herbal Medicine
- Herb & Oils Uses
- Herniated disk
- Home Remedies
- House Plants
- Humalog®
- Hydrogen Peroxide
- Hyperglycemia
- Hypoglycemia
- Hyperkalemia
- Hypokalemia
- Hypertension
- Hypotension
- Important Numbers
- Insomnia
- Insulin
- Juice Recipes
- Karma
- Kidney Cysts
- Kidney Disease
- Kinds of Tea
- Lantus®
- Lemon Cleanse
- Logger vs Lineman
- Macaroni!!
- Medicare
- Mental Health
- MO HealthNet
- Moon Phases
- Mounjaro®
- MRI Scan
- My Athletic Shoes
- My Boots & Spurs
- My Cowboy Hats
- Myelography
- Mystical Unicorn
- Nasal Polyps
- Natal Astrology Chart
- Never Forget
- Nuclear Medicine
- Nutrition - Adults
- Nutrition - Adults, Older
- Nutrition - Kids
- Obesity
- One Little Rose
- Orchid Growing
- Orchid Sources
- Pagan Humor
- Pagans vs.Wiccans
- Parking Spaces
- PayPal.Me
- Pentagram vs. Pentacle
- Perennials
- Peripheral Artery Disease
- PET/CT Scan
- PET Scan
- Phobias A-Z
- Plant Care
- Plant Zone Map
- Potassium
- Propagating Plants
- Prurigo Nodularis
- Psychic Gifts
- PVC's
- Quit Smoking
- Recipes I like
- Red Yeast Rice
- Roses
- Runes
- Sadie & Beethoven
- Salt & Sodium
- Salt Water Flush
- Sciatica
- Service Animals
- Shape Shifters
- Sleep Apnea
- Sleep Disorders
- Sleep Studies
- Smile
- SPECT Scan
- Speed Test
- Spices You Need
- Spices I Have
- Spinal Stenosis
- Stents
- Steel Toe vs. Comp. Toe
- Stress Test - Exercise
- Stress Test - Nuclear
- Sugars - Sweeteners
- Superstitions
- Symbols
- Tarot
- The Ten Commandments
- Tools of the Craft
- Top Expensive Movies
- Top Modern Westerns
- Top 100 Westerns
- Toyota Yaris 2008
- Toyota Yaris 2012
- Trazodone
- Tree, Calamondin Orange
- Tree, Lemon (Meyer)
- Tree, Lime
- Tree Signs
- Ultrasound
- US Bill of Rights
- US Constitution
- US Declaration of Independence
- Vaccines by Age
- Vaccines 0-6 yrs
- Vaccines 7-18 yrs
- Vaccines 19 and up
- Ventricular Fibrillation
- Vertigo
- Vital Records
- Vital Signs
- Vitamin B12
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin K
- Vitamins & Minerals
- Water Therapy
- Weight on other Planets
- Wiccan Rede
- X-Rays
- Yin / Yang
- Zodiac Signs
Needed to read PDF's
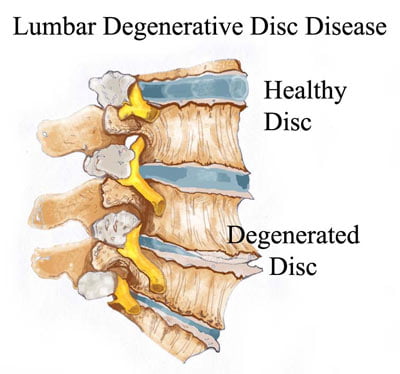
Degenerative Disk Disease
Overview
Degenerative disc disease (DDD) is a common condition in which the intervertebral discs in the spine break down and deteriorate, usually due to age-related wear and tear. The intervertebral discs act as cushions between the vertebrae in the spine, helping to absorb shock and allow the spine to move freely. In degenerative disc disease, these discs may become thinner, weaker, or less flexible, which can cause pain and stiffness. Treatment for degenerative disc disease may include medications, physical therapy, and, in some cases, surgery.
What is degenerative disk disease?
Degenerative disc disease (DDD) is a condition in which the intervertebral disc deteriorates and becomes thinner, weaker, and less flexible.
The spine is made up of a series of bones called vertebrae, which are stacked on top of each other and separated by intervertebral discs. These discs are made up of a tough, outer layer called the annulus fibrosus and a softer, gel-like center called the nucleus pulposus.
The intervertebral discs serve several important functions in the spine. They act as cushions between the vertebrae, helping to absorb shock and allowing the spine to move freely. They also help to distribute weight and load evenly across the spine.
In degenerative disc disease, the gel-like nucleus can dry out and the fibrous outer layer can become brittle, causing the disc to shrink or break down.What are spinal disks?
Spinal disks are like shock absorbers between the vertebrae, or bones, of your spine. They help your back stay flexible so you can bend and twist. As you get older, they can show signs of wear and tear. They begin to break down and may not work as well.
Nearly everyone's disks break down over time, but not everyone feels pain. If worn-out spinal disks are the reason you're hurting, you have degenerative disk disease.When the cushions wear away, the bones can start to rub together. This contact can cause pain and other problems, like:
- Adult scoliosis, where your spine curves
- Herniated disk, also called a bulged, slipped or ruptured disk
- Spinal stenosis, when the space in your spinal canal narrows
- Spondylolisthesis, when vertebrae move in and out of place
Types of degenerative disk disease
Disk degeneration mostly affects your lower back (lumbar spine) or neck (cervical spine).
- Lumbar degenerative disk disease. Your lower back (lumber spine) has five vertebrae. These are the largest bones in your back. Healthcare providers call them L1 to L5. Disks in your spine (spinal disks) separate each of these vertebrae. Approximately 90% of degenerative disk disease occurs in the lowest portions of your lumbar spine.
- Cervical degenerative disk disease. This type of degenerative disk disease occurs in the seven vertebrae of your neck (cervical spine). These vertebrae are each separated by a spinal disk. Your cervical spine is responsible for all kinds of movements, including looking up and down and turning your head from side to side. Degenerative disk disease in this area can make those movements painful.
- Multilevel degenerative disk disease. Multilevel degenerative disk disease is when degenerative disk disease affects more than one disk or level of your spine. So, areas of your lumbar spine and your cervical spine could be affected.
How common is degenerative disk disease?
Almost everyone has some disk degeneration after age 40, even if they don’t develop symptoms. It can lead to back pain in about 5% of adults. Degenerative disc disease is a common condition and its prevalence increases with age. By the age of 20, 37% of people show signs of disc degeneration on imaging. By the age of 70, that number increases to 93%.
Symptoms and Causes
Symptoms of degenerative disk disease
The most common degenerative disk disease (degenerative disc disease) symptoms are neck pain and back pain.
You may experience:
- Pain: Pain is the most common symptom of degenerative disc disease. It can range from a dull ache to a sharp, shooting pain. The pain may be worse when sitting, standing, or walking for long periods of time. It may also be worse when bending, lifting, or twisting the back.
- Stiffness: People with degenerative disc disease may experience stiffness in the back or neck. This may be worse in the morning or after periods of inactivity.
- Limited range of motion: Degenerative disc disease may cause difficulty with certain movements, such as bending, twisting, or reaching
- Weakness: Some people with degenerative disc disease may experience weakness in their legs or arms if there is associated nerve compression.
- Numbness or tingling: Degenerative disc disease may cause numbness or tingling in the arms, hands, legs, or feet if there is associated nerve compression.
Degenerative disk disease causes
Spinal disks wear down as a natural part of aging. Especially after age 40, most people experience some disk degeneration. But not everyone experiences pain.
You might have pain if your spinal disks:
- Dry out. When you're born, the disks in your spine are mostly made up of water. As you age, they lose water and get thinner. Flatter disks can't absorb shocks as well. The water loss also means less cushion or padding between your vertebrae. This can lead to other problems in your spine that may cause pain.
- Tear or crack. Stress and strain on your back can cause tiny tears in the outer wall of your disks, which contain nerves. Any tears near the nerves can become painful. And if the wall breaks down, the disk's soft core may push through the cracks. The disk may bulge, or it may slip out of place, which is called a slipped or herniated disk. It can affect nearby nerves.
Such tears can be caused by:
- Daily activities. Wear and tear on your back from the things you do every day, like lifting a heavy laundry basket, picking up a crying child, and working in the garden, can contribute to disk degeneration over time.
- Injuries. Even minor injuries to your back -- from a fall, for example, or lifting something heavy incorrectly -- make disk degeneration more likely. You may not feel pain at the time of the injury, but their impacts add up over time.
Risk factors for degenerative disk disease
Degenerative disk disease is most common in people age 40 and older.
Some factors increase your risk of developing degenerative disk disease, including:
- Aging. This is the big one. As you get older, your disks begin to degenerate. Some experts estimate that about 9 out of 10 people will show signs of disk degeneration by age 60. But that’s considered normal, and it does not always cause pain or other symptoms. If you do have symptoms, you likely have degenerative disk disease.
- Obesity. Several studies have linked being overweight to spinal damage, including degenerative disk disease. Excess weight puts stress on all parts of your spine. If you have obesity and carry the bulk of your weight in your middle, your risk of degenerative disk disease may be particularly high.
- Family history. Did one or both of your parents have degenerative disk disease? If so, you may be at higher risk because it can run in families. Scientists have identified many genes that may increase your risk.
- Smoking. Need another reason to quit? Several studies have reported that smoking ups your odds of degenerative disk disease. But that’s not all. If you already have degenerative disk disease, smoking may make it worse. You may feel more pain. If you need surgery, smoking may make you more likely to have complications.
- Heavy lifting and manual labor. Some research suggests that jobs in which you have to do a lot of heavy lifting may modestly bump up your risk of disk degeneration.
Does degenerative disk disease increase my risk for other conditions?
Degenerated disks can increase your risk of developing other spinal conditions.
Common spine problems include:
- Osteoarthritis
- Scoliosis
- Spinal stenosis
- Spondylolisthesis
- Radiculopathy
- Spondylolysis
Diagnosis and Tests
How doctors diagnose degenerative disk disease
To diagnose degenerative disk disease (degenerative disc disease), your healthcare provider may start by asking you about your symptoms.
Questions may include:
- When did the pain start?
- Where do you feel pain?
- What activities cause the most pain?
- What activities decrease the pain?
- Did you have an injury or accident that led to pain?
- Do you have other symptoms, like tingling or numbness?
- How far can you walk?
Your healthcare provider may use imaging scans, like X-ray, CT or MRI to help with the diagnosis of degenerative disk disease. These tests can show your healthcare provider the state and alignment of your disks.
Your provider may also conduct a physical exam to check your:
- Nerve function. Your provider may use a reflex hammer to check your reactions. Little or no reaction could mean you have damaged or compressed nerves.
- Pain levels. Your provider may touch or press on specific areas of your back to measure your pain levels.
- Strength. Muscle weakness or shrinking (atrophy) could mean you have nerve damage or degenerated disks.
What are the stages of degenerative disk disease?
Healthcare providers use the following four stages when diagnosing degenerative disk disease:
- Dysfunction. Your spinal disks have started to degenerate, and you may be experiencing mild degenerative disk disease.
- Dehydration. Your spinal disks have started to dry out, causing them to lose some of their height and flexibility. Your neck and back pain may worsen at this stage.
- Stabilization. At this stage, your spine tries to stabilize itself, which can cause spinal stenosis and severe pain.
- Collapse. Your spinal disks continue shrinking and the bones in your spine rub together. The damaged disks press against your nerves, causing severe pain.
Management and Treatment
How do you treat degenerative disk disease?
Usually, your healthcare provider will recommend noninvasive degenerative disk disease treatment options first.
Your treatment may include:
- Physical therapy. Physical therapy can help strengthen the muscles of the back and improve flexibility and range of motion. A physical therapist may also teach you exercises to help reduce pain and improve posture.
- Medication. Over-the-counter pain relievers like aspirin and ibuprofen can help fight inflammation. They can ease your pain and lessen swelling. Your doctor may prescribe a stronger drug for pain if you need it. Degenerative disk disease may also lead to muscle spasms. Your doctor may suggest medicine to help relieve them.
- Steroid shots. Corticosteroid injections around an irritated nerve can decrease inflammation and improve pain. Other newer therapies, such as plasma injections, can be injected directly into the intervertebral discs. These also include Growth Factors and Stem Cells that decrease inflammation and delay degeneration.
- Radiofrequency neurotomy. In this procedure, your doctor will use radio waves to heat and destroy nerve tissues in your spine. This prevents the nerve from sending pain signals to your brain. You may feel immediate pain relief, though it could take up to 3 weeks for the benefits to fully kick in. That pain relief typically lasts 6 months to a year, though it can continue for several years. Unfortunately, some people do not benefit as much as others from this procedure.
- Surgery. In severe cases of degenerative disc disease that do not respond to other treatments, surgery may be necessary. Options may include disc removal or replacement (discectomy), spinal fusion, or laminectomy (removal of a portion of the vertebrae to relieve pressure on the nerves).
It’s important to note that treatment options may vary depending on the individual’s specific condition and overall health. It’s important to discuss all treatment options with a doctor to determine the best course of treatment for your needs.
Degenerative disk disease self-care
Some people find pain relief through at-home remedies. At-home treatments may decrease pain for a short time. But they’re not a long-term treatment for severely degenerated disks.
You may try:
- Slim down. Excess weight strains your back and raises your odds of nerve damage and pain. Losing weight can help prevent or ease your discomfort.
- Get a massage. Some research suggests that massages can offer temporary lower back pain relief. Massage may be included in your physical therapy plan.
- Try TENS.Transcutaneous electrical nerve stimulation, or TENS, is a treatment that delivers small electrical impulses to your body to help ease pain. The treatment shouldn't feel painful, but more like a tingling sensation. You can buy a TENS device over-the-counter and use it at home. Ask your doctor to help you pick out the right TENS device for you and to show you how to use it.
- Correct your posture. By sitting and standing with a proper posture, you keep your spine in alignment and ease its workload. That can help prevent back pain. Your physical therapist may give you exercises to improve your posture.
- Exercise regularly. Lots of different types of exercise can help ease your back pain. These include yoga, tai chi, Pilates, and stretching. Talk to your doctor before you begin a new exercise program.
- Try hot and cold therapy. Apply a heating pad for 10 to 15 minutes to your back, then swap it out for a cold pack for another 10 to 15 minutes. Do this three to four times daily to ease pain and inflammation.
Degenerative disk disease surgery
Most people don’t need surgery for degenerative disk disease. But if you’ve tried multiple nonsurgical treatments and have persistent pain and/or weakness, surgery may be a good option.
Your surgeon may use one of a few types of spinal decompression surgery:
- Diskectomy: Part of the degenerated disk is removed. This relieves pressure on the nerves, easing pain, numbness, and weakness.
- Foraminotomy: During these procedures, the surgeon removes a portion of bone in your back in order to reach the problem disk and cut out the damaged portion to relieve pressure on the nerves. You may undergo a combination of these procedures.
- Artificial disk replacement. Your surgeon will remove the disk that’s causing your pain and replace it with a disk made of metal or metal and plastic.
- Spinal fusion: In this procedure, the damaged disk is removed and replaced by bone that connects to the bones above and below where the disk used to be. This eases pain and helps your back work better.
Prevention
How can I prevent degenerative disk disease from getting worse?
You can prevent or slow the progression of spinal degeneration through lifestyle changes.
Some of these include:
- Smoking. As mentioned earlier, smoking can worsen your pain. It also can make treatment for degenerative disk disease less effective.
- Heavy lifting. Lifting heavy weights puts strains and stresses the disks in your back, especially when done frequently, such as for work.
- Overdoing it with alcohol. Excessive drinking raises your risk of back pain.
- Sitting for long periods. Your back will feel better when walking rather than spending too much time at your desk or on your couch.
- High impact exercise. Exercises and sports that involve running, jumping, twisting, and other high-impact movements -- think football, weightlifting, tennis -- can be hard on your back. Try low impact exercises like walking and swimming instead.
Prognosis
Can you fully recover from degenerative disk disease?
Most people who have surgery for degenerative disk disease experience long-term pain relief. But even after surgery, you need to continue exercising and stretching to keep your back strong and healthy.
Many people use nonsurgical and at-home treatments to manage pain long term. If you have mild to moderate back pain, you’ll need to continue treatment to keep the pain at bay.
Additional Common Questions
How serious is degenerative disk disease?
Disks degenerate as you age. It’s a natural part of getting older, and you may not develop symptoms. But the degeneration can cause severe, even disabling pain. See your doctor if you develop any of the symptoms mentioned above.
What can be done for degenerative disk disease?
Lifestyle changes, such as weight loss and exercise, can ease your symptoms. Ibuprofen, aspirin, and other over-the-counter pain relievers also can help, as can steroid anesthetic shots. Your doctors have other treatments, including surgery, in their toolbox.
What triggers degenerative disk disease?
Lots of things up your odds of degenerative disk disease, but older age is the main risk factor. Most people over 60 show some signs of disk degeneration. Back injuries, even minor ones, and activities that put strain on your back can add up over time and contribute to degenerative disk disease. So can obesity. And, finally, if it runs in your family, degenerative disk disease may be in your future.
What are the four stages of degenerative disk disease?
- Dysfunction. The disks have begun to degenerate, and you may develop mild to moderate pain.
- Dehydration. At this stage, your spinal disks begin to dry out. This causes them to lose flexibility and some of their height. Your pain may worsen at this stage and become an everyday experience.
- Stabilization. Your spine attempts to stabilize itself. This can lead to spinal stenosis and more severe pain.
- Collapse. As the disks continue to shrink, the bones in your spine rub together and the damaged disks press against nerves. This causes severe pain.
What questions should I ask my healthcare provider?
You may want to ask your healthcare provider:
- What’s the most likely cause of my degenerative disk disease?
- How can I slow the progression of the disease?
- What nonsurgical treatments are most likely to relieve my pain?
- What will happen if I choose not to have surgery?
- How can I prevent pain from returning after surgery?
One Final Note..
Degenerative disk disease is a condition where your spinal disks break down with age and daily activity. Unfortunately, it’s just a natural part of aging. When these disks wear out, you’ll typically experience back pain and stiffness. Regular, low-impact exercise like swimming or yoga can help prevent the onset or slow the progression of the condition. While there are many nonsurgical and at-home treatments you can take to manage your pain, surgery may be necessary for long-term relief. Talk with your doctor to figure out the best treatment plan for you.
Find me on Social Media
 |
Don't forget to bookmark me to see updates.. Copyright © 2000 - 2025 K.
Kerr |







