- Main Page
- A1C Test
- Advance Directives
- Age on other Planets
- Aliens
- American Flag
- Annuals
- Anxiety
- Aortic Aneurysm
- Apple Cider Vinegar
- Arrhythmia
- Atrial Fibrillation
- Avoiding Scams
- Awareness Ribbons
- Bamboo
- Banana Tree, Grand Nain
- Banana Tree, Ice Cream
- Banana Tree, Zebrina Rojo
- Beekeeping
- Benign P P Vertigo
- Birth Month
- Blood Tests
- Blood Types
- Body Mass Index - BMI
- BMI Calculator
- Boogaloo
- Bookmarks
- Boot Anatomy
- Boot Fit Guide
- Boot Glossary
- Boot Leathers
- Boot Makers
- Boot Retailers
- Boot Styles - Western
- Boot Toes & Heels - Western
- Boot Toes & Heels - Work
- Bronchitis
- Candle Colors
- Carbohydrates
- Cardiac Catheterization
- Cardiovascular Disease
- CGM's
- Chakras
- Chinese Zodiac
- Cholesterol
- Christmas Tree
- Color Codes Chart
- C.O.P.D.
- Coronary Artery Disease
- Country Stars
- Cowboy Hat Etiquette
- Cowboy Hat Sizing
- C.P.A.P.
- Credit Score Checkers
- Crystals & Gems
- CT scan
- Degenerative Disk Disease
- Depression
- Diabetes Info.
- Diabetes Facts
- Diabetes - Pre
- Diabetes - Type 1
- Diabetes - Type 2
- Diabetes - Type 3c
- Diabetes - Gestational
- Diabetes Care
- Diabetes Care Team
- Diabetes Terms
- Diabetes Treatment
- Diabetes & Fruits
- Diabetes & Veg's
- Diet - Boiled Egg
- Diet - DASH
- Diet - Fat Burning
- Diet - Mediterranean
- Diet - Military
- Disability
- Do Not Resuscitate
- Dream Catchers
- Dupixent®
- Echocardiogram
- Electrocardiogram
- Emphysema
- Epsom Salt
- Eye Teasers
- Fairies
- Farxiga®
- Flower Astrology
- Fonts
- Foods To Regrow
- Friend
- Funny Things
- Fun Stuff
- Glycemic Index
- Gout
- Growing Blueberries
- Halloween
- Halloween Treats
- Headaches
- Health Info. Lines
- Heart Attack
- Heart Disease - Other
- Heart Failure
- Heart Tests
- Hello!!
- Herbal Codes
- Herbal Medicine
- Herb & Oils Uses
- Herniated disk
- Home Remedies
- House Plants
- Humalog®
- Hydrogen Peroxide
- Hyperglycemia
- Hypoglycemia
- Hyperkalemia
- Hypokalemia
- Hypertension
- Hypotension
- Important Numbers
- Insomnia
- Insulin
- Juice Recipes
- Karma
- Kidney Cysts
- Kidney Disease
- Kinds of Tea
- Lantus®
- Lemon Cleanse
- Logger vs Lineman
- Macaroni!!
- Medicare
- Mental Health
- MO HealthNet
- Moon Phases
- Mounjaro®
- MRI Scan
- My Athletic Shoes
- My Boots & Spurs
- My Cowboy Hats
- Myelography
- Mystical Unicorn
- Nasal Polyps
- Natal Astrology Chart
- Never Forget
- Nuclear Medicine
- Nutrition - Adults
- Nutrition - Adults, Older
- Nutrition - Kids
- Obesity
- One Little Rose
- Orchid Growing
- Orchid Sources
- Pagan Humor
- Pagans vs.Wiccans
- Parking Spaces
- PayPal.Me
- Pentagram vs. Pentacle
- Perennials
- Peripheral Artery Disease
- PET/CT Scan
- PET Scan
- Phobias A-Z
- Plant Care
- Plant Zone Map
- Potassium
- Propagating Plants
- Prurigo Nodularis
- Psychic Gifts
- PVC's
- Quit Smoking
- Recipes I like
- Red Yeast Rice
- Roses
- Runes
- Sadie & Beethoven
- Salt & Sodium
- Salt Water Flush
- Sciatica
- Service Animals
- Shape Shifters
- Sleep Apnea
- Sleep Disorders
- Sleep Studies
- Smile
- SPECT Scan
- Speed Test
- Spices You Need
- Spices I Have
- Spinal Stenosis
- Stents
- Steel Toe vs. Comp. Toe
- Stress Test - Exercise
- Stress Test - Nuclear
- Sugars - Sweeteners
- Superstitions
- Symbols
- Tarot
- The Ten Commandments
- Tools of the Craft
- Top Expensive Movies
- Top Modern Westerns
- Top 100 Westerns
- Toyota Yaris 2008
- Toyota Yaris 2012
- Trazodone
- Tree, Calamondin Orange
- Tree, Lemon (Meyer)
- Tree, Lime
- Tree Signs
- Ultrasound
- US Bill of Rights
- US Constitution
- US Declaration of Independence
- Vaccines by Age
- Vaccines 0-6 yrs
- Vaccines 7-18 yrs
- Vaccines 19 and up
- Ventricular Fibrillation
- Vertigo
- Vital Records
- Vital Signs
- Vitamin B12
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin K
- Vitamins & Minerals
- Water Therapy
- Weight on other Planets
- Wiccan Rede
- X-Rays
- Yin / Yang
- Zodiac Signs
Needed to read PDF's
Coronary Artery Disease
(CAD)
Overview
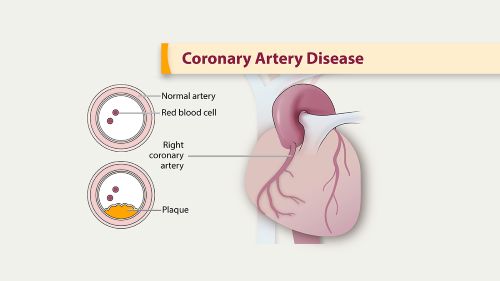
Coronary artery disease (CAD) limits blood flow in your coronary arteries, which deliver blood to your heart muscle. Cholesterol and other substances make up plaque that narrows your coronary arteries. Chest pain is the most common CAD symptom. CAD can lead to a heart attack, abnormal heart rhythms or heart failure. Many treatments are available.
What is coronary artery disease?
Coronary artery disease (CAD) is a narrowing or blockage of your coronary arteries, which supply oxygen-rich blood to your heart. This happens because, over time, plaque (including cholesterol) buildup in these arteries limits how much blood can reach your heart muscle.
Picture two traffic lanes that merge into one due to construction. Traffic keeps flowing, just more slowly. With CAD, you might not notice anything is wrong until the plaque triggers a blood clot. The blood clot is like a concrete barrier in the middle of the road. Traffic stops. Similarly, blood can’t reach your heart, and this causes a heart attack.
You might have CAD for many years and not have any symptoms until you experience a heart attack. That’s why CAD is a “silent killer.”
Other names for CAD include Coronary Artery Disease, Congenital Heart Disease, and ischemic heart disease. It’s also what most people mean when they use the general term “heart disease.”
Coronary artery disease types
There are three types of coronary artery disease:
- Obstructive coronary artery disease: This type occurs when a fatty substance called plaque builds up the coronary arteries, leading to artery narrowing. It's the most common type of coronary heart disease.
- Nonobstructive coronary artery disease: There's no plaque buildup in the coronary arteries. Instead, narrowing in the coronary artery is caused by other conditions, including irregular constrictions (coronary vasospasm), heart tissue that compresses the coronary arteries (myocardial bridging) or damage to the artery lining (endothelial dysfunction).
- Spontaneous coronary artery dissection (SCAD): A sudden tear in the coronary artery wall blocks blood flow to the heart. SCAD causes sudden symptoms that often present as a heart attack
How common is coronary artery disease?
Coronary artery disease is very common. Over 18 million adults in the U.S. have coronary artery disease. That’s roughly the combined populations of New York City, Los Angeles, Chicago and Houston.
In 2021, coronary artery disease killed 375,500 people in the U.S.
IN 2022, coronary artery disease killed 371,506 people in the U.S
About 1 in 20 adults age 20 and older have CAD (about 5%)
In 2022, about 1 out of every 5 deaths from cardiovascular diseases (CVDs) was among adults younger than 65 years old.
Symptoms and Causes
When you have coronary artery disease, plaque builds up in the arteries that supply blood to your heart, leading to the formation of blood clots.
What are the symptoms?
You may have no symptoms of coronary artery disease for a long time. Plaque buildup takes many years, even decades. But as your arteries narrow, you may notice mild symptoms. These symptoms mean your heart is pumping harder to deliver oxygen-rich blood to your body.
Symptoms of chronic CAD include:
- Chest pain, called angina. You may feel squeezing, pressure, heaviness, tightness or pain in the chest. It may feel like somebody is standing on your chest. The chest pain usually affects the middle or left side of the chest. Activity or strong emotions can trigger angina. There are different types of angina. The type depends on the cause and whether rest or medicine makes symptoms better. In some people, especially women, the pain may be brief or sharp and felt in the neck, arm or back.
- Shortness of breath (dyspnea): Some people feel short of breath during light physical activity.
- Fatigue. If the heart can't pump enough blood to meet your body's needs, you may feel unusually tired.
Sometimes, the first coronary artery disease symptom is a heart attack.
What causes coronary artery disease?
Atherosclerosis causes coronary artery disease. Atherosclerosis is the gradual buildup of plaque in arteries throughout your body. When the plaque affects blood flow in your coronary arteries, you have coronary artery disease.
Plaque consists of cholesterol, waste products, calcium and fibrin (a substance that helps your blood clot). As plaque collects along your artery walls, your arteries become narrow and stiff.
Plaque can clog or damage your arteries, which limits or stops blood flow to a certain part of your body. When plaque builds up in your coronary arteries, your heart muscle can’t receive enough blood. So, your heart can’t get the oxygen and nutrients it needs to work properly (myocardial ischemia). It leads to chest discomfort (angina) and puts you at risk of a heart attack.
People who have plaque buildup in their coronary arteries often have buildup elsewhere in their body, too. This can lead to conditions like carotid artery disease and peripheral artery disease (PAD).
Some causes of atherosclerosis and coronary artery disease are:
Diabetes or insulin resistance.
High blood pressure.
Lack of exercise.
Smoking or tobacco use.
Is it genetic?
Partly. Family history affects your risk of coronary artery disease, but many other risk factors have nothing to do with your genetics. The choices you make every day add up to a big impact on your risk of CAD.
What are the risk factors for coronary artery disease?
There are many risk factors for coronary artery disease. You can’t change all of them, but you can manage some of them by making lifestyle changes or taking medications. Talk with your provider about what you can do about these risk factors:
- Birth sex. Men are generally at greater risk of coronary artery disease. However, the risk for women increases after menopause.
- Family history. A family history of heart disease makes you more likely to get coronary artery disease. This is especially true if a parent, brother, sister or child got heart disease at an early age. The risk is highest if your father or a brother had heart disease before age 55 or if your mother or a sister developed it before age 65.
- Obesity. Too much body fat is bad for overall health. Obesity can lead to type 2 diabetes and high blood pressure. Ask your healthcare team what a healthy weight is for you.
- Not getting enough exercise. Physical activity is important for good health. A lack of exercise is linked to coronary artery disease and some of its risk factors.
- Alcohol use. Heavy alcohol use can lead to heart muscle damage. It also can worsen other risk factors of coronary artery disease
- Smoking. If you smoke, quit. Smoking is bad for heart health. People who smoke have a much greater risk of heart disease. Breathing in secondhand smoke also increases the risk.
- High blood pressure. Uncontrolled high blood pressure can make arteries hard and stiff. This can lead to atherosclerosis, which causes coronary artery disease.
- Cholesterol. Too much "bad" cholesterol in the blood can increase the risk of atherosclerosis. "Bad" cholesterol is called low-density lipoprotein (LDL) cholesterol. Not enough "good" cholesterol, called high-density lipoprotein (HDL) cholesterol, also leads to atherosclerosis.
- Unhealthy diet. Eating foods with a lot of saturated fat, trans fat, salt and sugar can increase the risk of coronary artery disease.
- A lot of stress. Emotional stress may damage the arteries and worsen other risk factors for coronary artery disease.
- Chronic kidney disease. Having long-term kidney disease increases the risk of coronary artery disease.
- Diabetes. Diabetes increases the risk of coronary artery disease. Type 2 diabetes and coronary artery disease share some risk factors, such as obesity and high blood pressure.
- Amount of sleep. Too little sleep and too much sleep both have been linked to an increased risk of heart disease.
Other possible risk factors for coronary artery disease may include:
- Breathing pauses during sleep, called obstructive sleep apnea. This condition causes breathing to stop and start during sleep. It can cause sudden drops in blood oxygen levels. The heart must work harder to pump blood. Blood pressure goes up.
- Increased high-sensitivity C-reactive protein (hs-CRP). This protein appears in higher than usual amounts when there's inflammation somewhere in the body. High hs-CRP levels may be a risk factor for heart disease. It's thought that as coronary arteries narrow, the level of hs-CRP in the blood goes up.
- High triglycerides. This is a type of fat in the blood. High levels may raise the risk of coronary artery disease, especially for women.
- High levels of homocysteine. Homocysteine is a substance that the body uses to make protein and to build and maintain tissue. But high levels of homocysteine may raise the risk of coronary artery disease.
- Preeclampsia. This pregnancy complication causes high blood pressure and increased protein in the urine. It can lead to a higher risk of heart disease later in life.
- Other pregnancy complications. Diabetes or high blood pressure during pregnancy are known risk factors for coronary artery disease.
- Certain autoimmune diseases. People who have conditions such as rheumatoid arthritis and lupus have an increased risk of atherosclerosis.
What are the complications of coronary artery disease?
The main complication of coronary artery disease is a heart attack. This is a medical emergency that can be fatal. Your heart muscle starts to die because it’s not receiving enough blood. You need prompt medical attention to restore blood flow to your heart and save your life.
Over the years, CAD can also weaken your heart and lead to complications, including:
- Irregular heart rhythms, called arrhythmias. If the heart doesn't get enough blood, changes in heart signaling can happen. This can cause irregular heartbeats. Some types of arrhythmias can be life-threatening.
- Chest pain, also called angina. Over time, coronary artery disease will cause plaque to build up inside your arteries and make them more narrow. As a result, your heart might not get enough blood when it needs it, such as during exercise, and you may feel chest pain and shortness of breath.
- Heart attack. This is the most common complication of coronary artery disease. Heart attacks occur when a piece of cholesterol plaque breaks off and causes a blood clot that blocks blood flow to the heart. The lack of blood damages the heart muscle, and if left untreated, a heart attack can be fatal. If you have symptoms of a heart attack, call 911.
- Heart failure. This is when your heart can’t pump enough blood. If you have narrowed arteries or high blood pressure, the walls of your heart might become weak or stiff, making it harder for your heart to work as well as it should.
In 2013–2016, 47% of men had high blood pressure, a major risk factor for heart disease and stroke.
More than 58.9 million women in the United States (45.7%) have high blood pressure (defined as 130/80 mm Hg or higher) or are taking blood pressure medicine. This includes almost 1 in 5 women of reproductive age.
Having high blood pressure increases the risk of developing heart disease and stroke and can lead to early death. High blood pressure is often underdiagnosed in women, and fewer than 1 in 4 women with high blood pressure (22.8%) have their condition under control.
Black women are nearly 60% more likely to have high blood pressure than White women. Pregnant women with high blood pressure have twice the risk of developing heart disease later in life compared to pregnant women without this condition. In the United States, high blood pressure develops in 1 in every 8 (13.0%) pregnancies.
Diagnosis and Tests
How is coronary artery disease diagnosed?
Healthcare providers diagnose coronary artery disease through a physical exam and testing.
During your physical exam, your provider will:
- Measure your blood pressure.
- Listen to your heart with a stethoscope.
- Ask what symptoms you’re experiencing and how long you’ve had them.
- Ask you about your medical history.
- Ask you about your lifestyle.
- Ask you about your family history. They’ll want to know about heart disease among your biological parents and siblings.
All of this information will help your provider determine your risk for heart disease.
What tests will be done?
Your provider may also recommend one or more tests to assess your heart function and diagnose CAD.
These include:
- Blood tests. Blood tests can check blood sugar and cholesterol levels. A high-sensitivity C-reactive protein (CRP) test checks for a protein linked to inflammation of the arteries.
- Cardiac catheterization and angiogram. This test can see blockages in the heart arteries. A doctor places a long, thin flexible tube called a catheter in a blood vessel, usually in the groin or wrist. It's guided to the heart. Dye flows through the catheter to arteries in the heart. The dye helps the arteries show up more clearly on X-ray images and video. Heart treatments may be done during this test.
- Coronary angioplasty. a procedure in which a expandable balloon is used to open up a narrowed artery. Nearly 90% of the time, a stent (metal scaffold) is placed at the site of the narrowing in the artery.
- Heart CT scan. A CT scan of the heart can show calcium deposits and blockages in the heart arteries. Calcium deposits can narrow the arteries. Sometimes dye is given by IV during this test. The dye helps create detailed pictures of the heart arteries. If dye is used, the test is called a CT coronary angiogram.
- Echocardiogram. This test uses sound waves to show blood flow through the heart. Parts of the heart that move weakly may be caused by a lack of oxygen or a heart attack. This may be a sign of coronary artery disease or other conditions.
- Electrocardiogram (ECG or EKG). This quick test checks the electrical activity of the heart. It shows how the heart is beating. Sticky patches called electrodes attach to the chest and sometimes the arms and legs. Wires connect the electrodes to a computer, which prints or displays the test results. The ECG signal patterns can show if you had or are having a heart attack.
- Nuclear stress test. This test shows how blood moves to the heart at rest and during activity. It uses a small amount of radioactive material, called a tracer or radiotracer. The substance is given by IV. An imaging machine takes pictures of how the tracer moves through the heart arteries. This helps find areas of poor blood flow or heart damage.
- Exercise stress test. If your symptoms usually occur during exercise, your healthcare professional may recommend this test. You walk on a treadmill or ride a stationary bike while your heart is checked. Because exercise makes the heart pump harder and faster than it does during most daily activities, an exercise stress test can show heart problems that might otherwise be missed. If you can't exercise, you may be given a medicine that affects the heart like exercise does. Sometimes an echocardiogram is done during an exercise stress test.
Management and Treatment
How is coronary artery disease treated?
Coronary artery disease treatment often includes lifestyle changes, risk factor management and medications. Some people may also need a procedure or surgery.
Your healthcare provider will talk with you about the best treatment plan for you. It’s important to follow your treatment plan so you can lower your risk of serious complications from CAD.
Lifestyle changes
Making certain lifestyle changes can help keep the arteries healthy and can prevent or slow coronary artery disease.
Such changes include:
- Don't smoke or use tobacco. Smoking is a major risk factor for coronary artery disease. Nicotine tightens blood vessels and forces the heart to work harder. Not smoking is one of the best ways to lower the risk of a heart attack. If you need help quitting, talk to your healthcare team.
- Eat heart-healthy foods. Choose plenty of fruits, vegetables and whole grains. Limit sugar, salt and saturated fats. Eating one or two servings of fish a week also may help keep the heart healthy.
- Get regular exercise. Exercise helps manage weight and control diabetes, cholesterol and blood pressure — all risk factors for coronary artery disease. Try to get 30 to 60 minutes of physical activity most days of the week. Ask your healthcare team what amount and type of exercise is best for you.Limit alcohol.
- Keep a healthy weight. Being overweight increases the risk of coronary artery disease. Losing even a small amount of weight can help reduce risk factors for coronary artery disease. Ask your healthcare team what the best weight is for you.
- Control blood pressure. Adults should get their blood pressure checked by a healthcare professional at least every two years. You may need to have checks more often if you have a history of high blood pressure. Ask your health professional what blood pressure goal is best for you.
- Get your cholesterol checked. Ask your healthcare team how often you need a cholesterol test. Lifestyle changes and medicines may be recommended to control cholesterol.
- Check your blood sugar. If you have diabetes, carefully managing your blood sugar can help reduce the risk of coronary artery disease.
- Avoid or limit alcohol. If you choose to drink alcohol, do so in moderation. For healthy adults, that means up to one drink a day for women and up to two drinks a day for men.
- Get good sleep. Poor sleep may increase the risk of heart disease and other chronic conditions. Adults should aim to get 7 to 9 hours of sleep daily.
- Manage stress. Find ways to help reduce emotional stress. Getting more exercise, practicing mindfulness and connecting with others in support groups are some ways to reduce stress.
Be sure to talk with your provider before starting any new exercise program. Your provider can also offer guidance on lifestyle changes tailored to your needs. They may recommend smoking cessation options or meeting with a dietitian to discuss healthy eating plans.
Risk factor management
Managing your risk factors for CAD can help slow down the progression of your disease. Work with your provider to manage the following conditions:
- Diabetes.
- High blood pressure.
- High cholesterol.
- High triglycerides (hypertriglyceridemia).
- Having a BMI higher than 25.
Medications
Medications can help you manage your risk factors and treat symptoms of coronary artery disease. Your provider may prescribe one or more medications that:
- Beta blockers. These medicines slow the heartbeat and lower blood pressure. If you've had a heart attack, beta blockers may reduce the risk of future heart attacks.
- Calcium channel blockers. One of these medicines may be suggested if you can't take beta blockers or beta blockers don't work for you. Calcium channel blockers can help reduce chest pain.
- Angiotensin-converting enzyme (ACE) inhibitors and angiotensin 2 receptor blockers (ARBs). These medicines lower blood pressure. They may help keep coronary artery disease from getting worse.
- Nitroglycerin. This medicine widens the heart arteries. It can help control or reduce chest pain. Nitroglycerin is available as a pill, spray or patch.
- Cholesterol medicine. Your healthcare professional might recommend this type of medicine to lower "bad" LDL cholesterol and reduce plaque buildup in the arteries. Such medicines include statins, niacin, fibrates and bile acid sequestrants.
- Ranolazine. This medicine may help people with long-term chest pain. It may be prescribed with or instead of a beta blocker.
- Aspirin. Aspirin helps thin the blood and prevent blood clots. Daily low-dose aspirin therapy may be recommended for the primary prevention of heart attack or stroke in some people. Daily use of aspirin can have serious side effects, including bleeding in the stomach and intestines. Don't start taking a daily aspirin without talking to your healthcare team.
Procedures and surgeries
Some people need a procedure or surgery to manage coronary artery disease, including:
- Coronary angioplasty and stent placement. This treatment opens clogged blood vessels in the heart. A tiny balloon on a thin tube, called a catheter, is used to widen a clogged artery and improve blood flow. A small wire mesh tube called a stent may be placed to keep the artery open. Most stents are coated with medicine that helps keep the artery open. This treatment also is called percutaneous coronary intervention.
- Coronary artery bypass graft (CABG) surgery. This is a type of open-heart surgery. During CABG, a surgeon takes a vein or artery from somewhere else in the body. The surgeon uses the blood vessel to create a new path for blood to go around a blocked or narrowed heart artery. The surgery increases blood flow to the heart.
- Atherectomy. A rotating shaver is used to remove plaque from the artery.
Cardiac rehabilitation: Cardiac rehabilitation is an important program for anyone recovering from a heart attack, heart failure, or other heart problem that required surgery or medical care. Cardiac rehab is a supervised program that includes:
- Physical activity.
- Education about healthy living, including healthy eating, taking medicine as prescribed, and ways to help you quit smoking.
- Counseling to find ways to relieve stress and improve mental health.
A team of people may help you through cardiac rehab, including your health care team, exercise and nutrition specialists, physical therapists, and counselors or mental health professionals.
Complications/side effects of the treatment
Complications or side effects of coronary artery disease treatments may include:
- Bleeding.
- Diarrhea.
- Dizziness.
- Cough.
- Blood clot.
- Coronary artery puncture.
- Infection.
- Abnormal heart rhythms.
- Cardiac tamponade.
How long does it take to recover from this treatment?
After PCI (angioplasty), you can usually get back to normal activities within a week. After CABG (bypass surgery), you’ll be in the hospital for more than a week. After that, it’ll take six to 12 weeks for a full recovery. If you've had coronary artery bypass surgery, your healthcare professional may suggest cardiac rehabilitation. This is a program of education, counseling and exercise training that's designed to help improve your health after heart surgery.
Prevention
Can coronary artery disease be prevented?
The lifestyle habits used to treat coronary artery disease also can help prevent it. A healthy lifestyle can help keep the arteries strong and clear of blockages. To improve heart health, follow these tips:
- Do not smoke or use tobacco.
- Limit or do not drink alcohol.
- Control blood pressure, cholesterol and diabetes.
- Exercise and stay active.
- Maintain a healthy weight.
- Eat a low-fat, low-salt diet that's rich in fruits, vegetables and whole grains.
- Reduce and manage stress.
- Get 7 to 9 hours of sleep daily.
Regular health checkups also are important. Some of the main risk factors for coronary artery disease — high cholesterol, high blood pressure and diabetes — have no symptoms in the early stages. Early detection and treatment can help you keep your heart healthy. Also ask about recommended vaccines, such as a yearly flu vaccine.
Prognosis
What can I expect if I have coronary artery disease?
Your provider is the best person to ask about your prognosis. Outcomes vary based on the person. Your provider will look at the big picture, including your age, medical conditions, risk factors and symptoms. Lifestyle changes and other treatments can improve your chances of a good prognosis.
Can coronary artery disease be reversed?
You can’t reverse coronary artery disease. But you can manage your condition and prevent it from getting worse. Work with your healthcare provider and follow your treatment plan. Doing so will give you the strongest possible chance of living a long and healthy life.
Living With CAD
How do I take care of myself?
The most important thing you can do is keep up with your treatment plan. This may include lifestyle changes and medications. It may also involve a procedure or surgery and the necessary recovery afterward.
Along with treatment, your provider may recommend cardiac rehab. A cardiac rehab program is especially helpful for people recovering from a heart attack or living with heart failure. Cardiac rehab can help you with exercise, dietary changes and stress management.
Coronary artery disease and mental health
A CAD diagnosis may make you think about your heart and arteries more than ever before. This can be exhausting and overwhelming. You may worry a lot about your symptoms or what might happen to you. Many people with coronary artery disease experience depression and anxiety. It’s normal to worry when you’re living with a condition that can be life-threatening.
But the worry shouldn’t consume your daily life. You can still live an active, fulfilling life while having heart disease. If your diagnosis is affecting your mental health, talk with a counselor. Find a support group where you can meet people who share your concerns. Don’t feel you need to keep it all inside or be strong for others. CAD is a life-changing diagnosis. It’s OK to devote time to processing it all and figuring out how to feel better, both physically and emotionally.
Living in the shadow of a potential heart attack or other heart problems can be unnerving—but it can also be motivating. Here’s what to focus on after a diagnosis.
Know your numbers. Heart health is in large part a numbers game. The key numbers to know include your HDL and LDL cholesterol, total cholesterol and triglycerides, your blood pressure, your glucose, your BMI and your waist circumference measurement, says McEvoy. Get your measurements and readings as often as recommended, make the recommended lifestyle changes and be sure to take medications as directed. This knowledge can be a powerful incentive.
Be optimistic. Fear of future cardiac events is common and natural. You may feel anxious, or even depressed. But with good medical care and personal effort, you can still lead a long life of high quality. Small changes really do add up.
When should I see my Cardiologist
Your provider will tell you how often you need to come in for testing or follow-ups.
You may have appointments with specialists (like a cardiologist) in addition to your primary care visits.Call your provider if you:
- Experience new or changing symptoms.
- Have side effects from your medication.
- Have questions or concerns about your condition or your treatment plan.
When should I go to the ER?
If you notice the symptoms of a heart attack in yourself or someone else, call 9-1-1 immediately. The sooner you get to an emergency room, the sooner you can get treatment to reduce the amount of damage to the heart muscle. At the hospital, health care professionals can run tests to find out if a heart attack is happening and can decide the best treatment.
In some cases, a heart attack requires cardiopulmonary resuscitation (CPR) or an electrical shock (defibrillation) to the heart to get the heart pumping again. Bystanders trained to use CPR or a defibrillator may be able to help until emergency medical personnel arrive.
Remember, the chances of surviving a heart attack are better the sooner emergency treatment begins.
What questions should I ask my Cardiologist?
If your provider hasn’t diagnosed you with coronary artery disease, consider asking:
- What are my risk factors for coronary artery disease?
- What can I do to lower my risk?
- What lifestyle changes are most important for me?
- What medications would lower my risk, and what are the side effects? How long do I need to stay on these medications?
If you have coronary artery disease, some helpful questions include:
- What can I do to slow down disease progression?
- What’s the best treatment plan for me?
- What lifestyle changes should I make?
- What medications do I need, and what are the side effects?
- Will I need a procedure or surgery? What does the recovery look like?
- Are there support groups or resources you can recommend?
What to expect from your Cardiologist?
A healthcare professional who sees you for coronary artery disease may ask:
- What are your symptoms?
- When did you begin having symptoms?
- Have the symptoms gotten worse over time?
- Do you have chest pain or difficulty breathing?
- If so, what does the chest pain feel like?
- Does exercise or activity make the symptoms worse?
- Does anyone in your family have a heart condition or high blood pressure?
- Have you been diagnosed with other health conditions?
- What medicines do you take?
- How much do you exercise in a typical week?
- What's your usual daily diet?
- Do you or did you smoke? How much? If you quit, when?
- Do you drink alcohol? How much?
CAD FAQs
What is the life expectancy of someone with coronary artery disease?The life expectancy of someone with CAD will vary, depending on their age, medical history, and lifestyle choices. If you’ve been diagnosed with coronary artery disease, talk with your doctor about your prognosis.
What are the coronary arteries?
There are two main coronary arteries. The left main coronary artery supplies blood to the left ventricle and left atrium, while the right coronary artery sends blood to the right ventricle, right atrium, and the sinoatrial and atrioventricular nodes. Both sides divide into smaller branches to supply blood to all parts of the heart.
One Final Note..
Coronary artery disease is a condition that restricts blood flow to your heart. It can be categorized as either atherosclerotic or nonatherosclerotic coronary artery disease. Obstructive coronary artery disease, the most common type, is caused by plaque buildup in your arteries. Nonobstructive coronary artery disease is caused by artery spasms and blood vessel irregularities. SCAD is caused by a tear in the layers of your coronary artery wall. Treatment of coronary artery disease may involve lifestyle strategies, medications, heart rehabilitation, and, in more serious cases, surgery.
Coronary artery disease is the most common form of heart disease in the U.S. If you've been diagnosed with the condition, your doctor will help you find the treatment plan that's right for you. Coronary artery disease can lead to serious complications, including heart attack and arrhythmia, but quitting smoking, eating a low-sodium diet, and maintaining a healthy weight are steps you can take right away to help lower your risk. Always talk with your doctor if your symptoms change, and ask them before making any major changes to your exercise routine.
Find me on Social Media
 |
Don't forget to bookmark me to see updates.. Copyright © 2000 - 2025 K.
Kerr |







