- Main Page
- A1C Test
- Advance Directives
- Age on other Planets
- Aliens
- American Flag
- Annuals
- Anxiety
- Aortic Aneurysm
- Apple Cider Vinegar
- Arrhythmia
- Atrial Fibrillation
- Avoiding Scams
- Awareness Ribbons
- Bamboo
- Banana Tree, Grand Nain
- Banana Tree, Ice Cream
- Banana Tree, Zebrina Rojo
- Beekeeping
- Benign P P Vertigo
- Birth Month
- Blood Tests
- Blood Types
- Body Mass Index - BMI
- BMI Calculator
- Boogaloo
- Bookmarks
- Boot Anatomy
- Boot Fit Guide
- Boot Glossary
- Boot Leathers
- Boot Makers
- Boot Retailers
- Boot Styles - Western
- Boot Toes & Heels - Western
- Boot Toes & Heels - Work
- Bronchitis
- Candle Colors
- Carbohydrates
- Cardiac Catheterization
- Cardiovascular Disease
- CGM's
- Chakras
- Chinese Zodiac
- Cholesterol
- Christmas Tree
- Color Codes Chart
- C.O.P.D.
- Coronary Artery Disease
- Country Stars
- Cowboy Hat Etiquette
- Cowboy Hat Sizing
- C.P.A.P.
- Credit Score Checkers
- Crystals & Gems
- CT scan
- Degenerative Disk Disease
- Depression
- Diabetes Info.
- Diabetes Facts
- Diabetes - Pre
- Diabetes - Type 1
- Diabetes - Type 2
- Diabetes - Type 3c
- Diabetes - Gestational
- Diabetes Care
- Diabetes Care Team
- Diabetes Terms
- Diabetes Treatment
- Diabetes & Fruits
- Diabetes & Veg's
- Diet - Boiled Egg
- Diet - DASH
- Diet - Fat Burning
- Diet - Mediterranean
- Diet - Military
- Disability
- Do Not Resuscitate
- Dream Catchers
- Dupixent®
- Echocardiogram
- Electrocardiogram
- Emphysema
- Epsom Salt
- Eye Teasers
- Fairies
- Farxiga®
- Flower Astrology
- Fonts
- Foods To Regrow
- Friend
- Funny Things
- Fun Stuff
- Glycemic Index
- Gout
- Growing Blueberries
- Halloween
- Halloween Treats
- Headaches
- Health Info. Lines
- Heart Attack
- Heart Disease - Other
- Heart Failure
- Heart Tests
- Hello!!
- Herbal Codes
- Herbal Medicine
- Herb & Oils Uses
- Herniated disk
- Home Remedies
- House Plants
- Humalog®
- Hydrogen Peroxide
- Hyperglycemia
- Hypoglycemia
- Hyperkalemia
- Hypokalemia
- Hypertension
- Hypotension
- Important Numbers
- Insomnia
- Insulin
- Juice Recipes
- Karma
- Kidney Cysts
- Kidney Disease
- Kinds of Tea
- Lantus®
- Lemon Cleanse
- Logger vs Lineman
- Macaroni!!
- Medicare
- Mental Health
- MO HealthNet
- Moon Phases
- Mounjaro®
- MRI Scan
- My Athletic Shoes
- My Boots & Spurs
- My Cowboy Hats
- Myelography
- Mystical Unicorn
- Nasal Polyps
- Natal Astrology Chart
- Never Forget
- Nuclear Medicine
- Nutrition - Adults
- Nutrition - Adults, Older
- Nutrition - Kids
- Obesity
- One Little Rose
- Orchid Growing
- Orchid Sources
- Pagan Humor
- Pagans vs.Wiccans
- Parking Spaces
- PayPal.Me
- Pentagram vs. Pentacle
- Perennials
- Peripheral Artery Disease
- PET/CT Scan
- PET Scan
- Phobias A-Z
- Plant Care
- Plant Zone Map
- Potassium
- Propagating Plants
- Prurigo Nodularis
- Psychic Gifts
- PVC's
- Quit Smoking
- Recipes I like
- Red Yeast Rice
- Roses
- Runes
- Sadie & Beethoven
- Salt & Sodium
- Salt Water Flush
- Sciatica
- Service Animals
- Shape Shifters
- Sleep Apnea
- Sleep Disorders
- Sleep Studies
- Smile
- SPECT Scan
- Speed Test
- Spices You Need
- Spices I Have
- Spinal Stenosis
- Stents
- Steel Toe vs. Comp. Toe
- Stress Test - Exercise
- Stress Test - Nuclear
- Sugars - Sweeteners
- Superstitions
- Symbols
- Tarot
- The Ten Commandments
- Tools of the Craft
- Top Expensive Movies
- Top Modern Westerns
- Top 100 Westerns
- Toyota Yaris 2008
- Toyota Yaris 2012
- Trazodone
- Tree, Calamondin Orange
- Tree, Lemon (Meyer)
- Tree, Lime
- Tree Signs
- Ultrasound
- US Bill of Rights
- US Constitution
- US Declaration of Independence
- Vaccines by Age
- Vaccines 0-6 yrs
- Vaccines 7-18 yrs
- Vaccines 19 and up
- Ventricular Fibrillation
- Vertigo
- Vital Records
- Vital Signs
- Vitamin B12
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin K
- Vitamins & Minerals
- Water Therapy
- Weight on other Planets
- Wiccan Rede
- X-Rays
- Yin / Yang
- Zodiac Signs
Needed to read PDF's
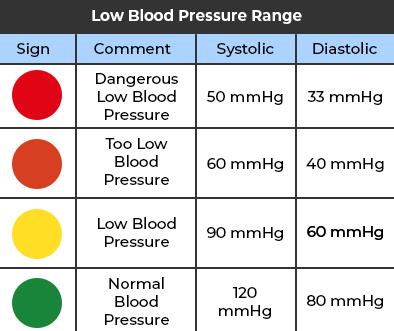
Hypotension
(Low Blood Pressure)
What is Low blood pressure?
Low blood pressure is a reading below 90/60 mm Hg. Many issues can cause low blood pressure. Treatment varies depending on what’s causing it. Symptoms of low blood pressure include dizziness and fainting, but many people don’t have symptoms. The cause also affects your prognosis.
Hypotension is the medical term for low blood pressure. You have it when a reading shows your blood pressure is much lower than expected. Other names include Hypotension; Blood pressure - low; Postprandial hypotension; Orthostatic hypotension; Neurally mediated hypotension; NMH
A blood pressure reading appears as two numbers. The top number is a measure of systolic pressure, or the pressure in the arteries when the heart beats and fills them with blood. The bottom number measures diastolic pressure, the pressure in the arteries when the heart rests between beats. The optimal blood pressure level is less than 120/80. (You may also see it written as 120/80 mmHg).Types of low blood pressure
Types of low blood pressure include:
- Postprandial hypotension. This drop in blood pressure occurs 1 to 2 hours after eating. It's most likely to affect older adults, especially those with high blood pressure. The risk also is higher for older adults with Parkinson's disease or other conditions that affect the part of the nervous system that controls automatic functions such as breathing and heart rate. This is called the autonomic nervous system. Certain lifestyle changes might help ease symptoms of postprandial hypotension. Eat small, low-carbohydrate meals, drink more water, and stay away from alcohol.
- Orthostatic hypotension, also called postural hypotension. This is a sudden drop in blood pressure when standing up after sitting or lying down. Causes include dehydration, long-term bed rest, pregnancy, certain medical conditions and some medicines. This type of low blood pressure is common in older adults.
- Neurally mediated hypotension. This is a blood pressure drop that happens after standing for long amounts of time. This type of low blood pressure mostly affects young adults and children. It might result from communication trouble between the heart and the brain.
- Multiple system atrophy with orthostatic hypotension. This rare condition affects the autonomic nervous system. Multiple system atrophy with orthostatic hypotension is linked with having very high blood pressure while lying down. It also used to be called Shy-Drager syndrome.
Measuring blood pressure involves two numbers:
- Systolic (top number): The top number is the pressure in the arteries when the heart beats.
- Diastolic (bottom number): The bottom number is the pressure in the arteries when the heart rests between beats.
Purchase a blood pressure monitor for yourself here at iHealth Labs Inc
Print a copy of the Blood Pressure Log for your use
What is considered low blood pressure?
Doctors consider you to have low blood pressure when your reading is less than 90/60.
The risk of both low and high blood pressure increases with age due in part to normal changes during aging.How common is low blood pressure?
Because low blood pressure is common without any symptoms, it’s impossible to know how many people it affects. However, orthostatic hypotension seems to be more and more common as you get older. An estimated 5% of people have it at age 50, while that figure climbs to more than 30% in people over 70.
Who does low blood pressure affect?
Hypotension can affect people of any age and background, depending on why it happens. However, it’s more likely to cause symptoms in people over 50 (especially orthostatic hypotension). It can also happen (with no symptoms) to people who are very physically active, which is more common in younger people.
Is low blood pressure serious?
In healthy people, low blood pressure without any symptoms isn't usually a concern and doesn't require treatment. But low blood pressure can be a sign of an underlying problem -- especially in older people -- and could reduce blood flow to the heart, brain, and other vital organs.
Long-lasting low blood pressure with no symptoms is almost never serious. But you can have health problems when your blood pressure drops suddenly and your brain doesn't have an adequate blood supply. This can lead to dizziness, lightheadedness, and sometimes fainting.
Types of low blood pressure
There are several types of low blood pressure:
- Orthostatic hypotension, also called postural hypotension. This is a sudden drop in blood pressure when standing up after sitting or lying down. Causes include dehydration, long-term bed rest, pregnancy, certain medical conditions and some medicines. This type of low blood pressure is common in older adults.
- Neurally mediated hypotension. This is a blood pressure drop that happens after standing for long amounts of time. This type of low blood pressure mostly affects young adults and children. It might result from communication trouble between the heart and the brain.
- Postprandial hypotension. This drop in blood pressure occurs 1 to 2 hours after eating. It's most likely to affect older adults, especially those with high blood pressure. The risk also is higher for older adults with Parkinson's disease or other conditions that affect the part of the nervous system that controls automatic functions such as breathing and heart rate. This is called the autonomic nervous system. Certain lifestyle changes might help ease symptoms of postprandial hypotension. Eat small, low-carbohydrate meals, drink more water, and stay away from alcohol.
- Multiple system atrophy with orthostatic hypotension. This rare condition affects the autonomic nervous system. Multiple system atrophy with orthostatic hypotension is linked with having very high blood pressure while lying down. It also used to be called Shy-Drager syndrome.
Symptoms and Causes
What are the symptoms of low blood pressure?
Low blood pressure symptoms include:
- Dizziness or feeling lightheaded.
- Fainting or passing out (syncope).
- Nausea or vomiting.
- Distorted or blurred vision.
- Fast, shallow breathing.
- Fatigue or weakness.
- Feeling tired, sluggish or lethargic.
- Confusion or trouble concentrating.
- Agitation or other unusual changes in behavior (a person not acting like themselves).
For people with symptoms, the effects depend on why hypotension is happening, how fast it develops and what caused it. Slow decreases in blood pressure happen normally, so hypotension becomes more common as people get older. A sudden fall in blood pressure can be dangerous. A change of just 20 mm Hg can make you feel dizzy or faint. For example, those symptoms could happen after a drop in systolic pressure from 110 mm Hg to 90 mm Hg. And big drops can be life-threatening. These can happen for reasons such as serious bleeding, serious infections or allergic reactions.
Usually, your body can automatically control your blood pressure and keep it from dropping too much. If it starts to drop, your body tries to make up for that, either by speeding up your heart rate or constricting blood vessels to make them narrower. Symptoms of hypotension happen when your body can’t offset the drop in blood pressure.
For many people, hypotension doesn’t cause any symptoms. Many people don’t even know their blood pressure is low unless they measure their blood pressure.
What are the possible signs of low blood pressure?
Your healthcare provider may observe these signs of low blood pressure:
- A heart rate that’s too slow or too fast.
- A skin color that looks lighter than it usually does.
- Cool kneecaps.
- Low cardiac output (how much blood your heart pumps).
- Low urine (pee) output.
What causes low blood pressure?
Hypotension can happen for a wide range of reasons. Causes of low blood pressure include:
- Orthostatic hypotension: This happens when you stand up too quickly and your body can’t compensate with more blood flow to your brain.
- Hormone-related diseases, also called endocrine conditions. Conditions such as Addison's disease that affect certain glands that make key hormones may cause blood pressure to drop. Low blood sugar, also called hypoglycemia, may lower blood pressure too. So might diabetes.
- Central nervous system diseases: Conditions like Parkinson’s disease can affect how your nervous system controls your blood pressure. People with these conditions may feel the effects of low blood pressure after eating because their digestive systems use more blood as they digest food.
- Dehydration. When the body doesn't have enough water, the amount of blood in the body declines. This can cause blood pressure to drop. Fever, vomiting, severe diarrhea, overuse of diuretic medicines and strenuous exercise can lead to dehydration.
- Life-threatening conditions: These conditions include irregular heart rhythms (arrhythmias), pulmonary embolism (PE), heart attacks and collapsed lung.
- Severe allergic reaction, also called anaphylaxis. Symptoms of a severe allergic reaction include a sudden and large drop in blood pressure.
- Heart and heart valve conditions: A heart attack, heart failure, heart valve disease and a slow heart rate called bradycardia can cause low blood pressure.
- Severe infection. When an infection in the body enters the bloodstream, it can lead to a life-threatening drop in blood pressure called septic shock. Another name for an infection that happens when germs get into the blood and spread is septicemia.
- Blood loss. Losing a lot of blood also reduces blood volume, leading to a severe drop in blood pressure. Causes of serious blood loss include injuries and internal bleeding.
- Prescription medications: Hypotension can happen with medications that treat high blood pressure, heart failure, erectile dysfunction, neurological problems, depression and more. Don’t stop taking any prescribed medicine unless your provider tells you to stop.
- Lack of nutrients in the diet. Low levels of vitamin B-12, folate and iron can keep the body from making enough red blood cells. A lack of healthy red blood cells is called anemia, and it can lead to low blood pressure.
- Alcohol or recreational drugs: Recreational drugs can lower your blood pressure, as can alcohol (for a short time). Certain herbal supplements, vitamins or home remedies can also lower your blood pressure. This is why you should always include these when you tell your healthcare provider what medications you’re taking.
- Pregnancy: Changes during pregnancy cause blood vessels to expand fast. The changes may cause blood pressure to drop. Low blood pressure is common in the first 24 weeks of pregnancy. After a person gives birth, blood pressure usually returns to the level that it was before pregnancy.
- Extreme temperatures: Being too hot or too cold can affect hypotension and make its effects worse.
What are the complications of low blood pressure?
Complications that can happen because of hypotension include:
- Falls and fall-related injuries: These are the biggest risks with hypotension because it can cause dizziness and fainting. Falls can lead to broken bones, concussions and other serious or even life-threatening injuries. If you have hypotension, preventing falls should be one of your biggest priorities.
- Shock: When your blood pressure is low, that can affect your organs by reducing the amount of blood they get. That can cause organ damage or even shock (where your body starts to shut down because of limited blood flow and oxygen).
- Heart problems or stroke: Low blood pressure can cause your heart to try to compensate by pumping faster or harder. Over time, that can cause permanent heart damage and even heart failure. It can also cause problems like deep vein thrombosis (DVT) and stroke because blood isn’t flowing like it should, causing clots to form.
Risk factors
Anyone can have low blood pressure. Risk factors for hypotension include:
- Age. Drops in blood pressure when standing up or after eating occur mainly in adults older than 65. Neurally mediated hypotension mainly affects children and younger adults.
- Medications. Certain medicines have the potential to cause low blood pressure. These include all medicines that treat high blood pressure.
- Certain diseases. Parkinson's disease, diabetes and some heart conditions can lead to low blood pressure.
- Alcohol or illegal drugs. Either of these may raise the risk of low blood pressure.
Diagnosis and Tests
To find out if you have low blood pressure, also called hypotension, your healthcare professional gives you a physical exam. You're also asked questions about your medical history. The exam includes checking your blood pressure.
You also can measure your blood pressure at home. Checking your blood pressure at home can help your healthcare professional diagnose high blood pressure earlier than usual.
Purchase a blood pressure monitor for yourself here at iHealth Labs Inc
Print a copy of the Blood Pressure Log for your use
Ask a member of your healthcare team to:
- Help you pick a blood pressure monitor.
- Tell you how often to check your blood pressure.
- Explain what blood pressure numbers should prompt you to call the medical office right away.
If you get a home blood pressure reading at or just below 90/60 mm Hg, it's not always a cause for concern. Your healthcare professional might tell you that the reading is OK for you, especially if you have no symptoms.
How is low blood pressure diagnosed?
Hypotension itself is easy to diagnose. Taking your blood pressure is all you need to do. But figuring out why you have hypotension is another story. If you have symptoms, a healthcare provider will likely use a variety of tests to figure out why it’s happening and if there’s any danger to you because of it.
What tests will be done to diagnose low blood pressure?
Your provider may recommend the following tests:
Lab testing
Tests on your blood and pee (urine) can look for any potential problems, like:
- Diabetes.
- Vitamin deficiencies.
- Thyroid or hormone problems.
- Low iron levels (anemia).
- Pregnancy (for anyone who can become pregnant).
Imaging
If providers suspect a heart or lung problem is behind your hypotension, they’ll likely use imaging tests to see if they’re right.
These tests include:
- X-rays.
- Computed tomography (CT) scans.
- Magnetic resonance imaging (MRI).
- Echocardiogram or similar ultrasound-based tests.
Diagnostic testing
These tests look for specific problems with your heart or other body systems.
- Electrocardiogram (ECG or EKG). This quick and painless test measures the electrical activity of the heart. During an ECG, sensors called electrodes are attached to the chest and sometimes to the arms or legs. Wires attached to the sensors connect to a machine that displays or prints out results. An ECG shows how fast or slow the heart is beating. It can be used to detect a current or previous heart attack.
- Exercise stress testing.
- Tilt table test. A tilt table test can study how the body reacts to changes in position. The test involves lying on a table that's tilted to raise the upper part of the body. This mimics the movement from lying down to standing up. Straps hold the body in place. Heart rate and blood pressure are tracked during the test.
Management and Treatment
How is low blood pressure treated?
Low blood pressure treatment usually starts with finding out why it’s happening. If a provider can treat that cause directly, hypotension will usually get better on its own. For example, hypotension can happen because of an injury and blood loss. Repairing that injury and replacing the lost blood with a blood transfusion will stop hypotension as long as the repair to the injury holds.
If you take medications that affect your blood pressure, your healthcare provider may change your dosage or have you stop taking that medication entirely.
If the cause remains a mystery, it’s also possible to treat it directly. However, curing hypotension is only possible if there’s an underlying cause that’s curable.
What medications and treatments are used?
Medications for low blood pressure
These drugs are sometimes used to treat low blood pressure:
- Fludrocortisone. This medication seems to help some types of low blood pressure. It works by promoting sodium retention by your kidneys. This causes fluid retention and some swelling, which is necessary to improve blood pressure. But sodium retention also causes a loss of potassium. So when taking fludrocortisone, make sure you get enough potassium each day. Fludrocortisone has none of the anti-inflammatory properties of cortisone or prednisone and doesn't build muscle like anabolic steroids.
- Midodrine. This drug activates receptors on your smallest arteries and veins to boost blood pressure. It's used to increase standing blood pressure in people who have postural hypotension related to problems with the nervous system.
The most important thing for a provider treating low blood pressure is to find the underlying cause and correct it. Treatments can range from simple IV fluids to antibiotics to surgery or even a heart transplant. Some people with low blood pressure need a hospital stay.
Treating hypotension directly usually happens in one of three ways:
- Increasing blood volume: This method, also known as fluid resuscitation, involves infusing fluids into your blood. Examples include intravenous (IV) fluids or plasma or blood transfusions.
- Making blood vessels constrict: Just as there are medications that lower your blood pressure by relaxing blood vessels in your body, there are also medications that have the opposite effect.
- Changing how your body handles fluids: Your kidneys are responsible for maintaining the fluid balance in your body. Certain medications can make your kidneys keep fluid and salt in your body, which can help with low blood pressure.
If the cause of low blood pressure isn't clear or if no treatment exists, the goal is to raise blood pressure and relieve symptoms. Depending on your age, health and the type of low blood pressure you have, there are various ways to do this:
- Use more salt. Experts usually recommend limiting table salt and foods high in sodium. That's because salt and sodium can raise blood pressure, sometimes by a lot. For people with low blood pressure, though, that can be a good thing. But too much salt or sodium can lead to heart failure, especially in older adults. So it's important to check with a healthcare professional before eating more salt or high-sodium foods.
- Drink more water. Fluids increase blood volume and help prevent dehydration, both of which are important in treating hypotension.
- Wear compression stockings. Also called support stockings, these elastic stockings are often used to relieve the pain and swelling of varicose veins. They improve blood flow from the legs to the heart. Some people have an easier time using compression belts around the stomach area than they do using compression stockings. The compression belts are called abdominal binders.
- Medicines. Various medicines can treat low blood pressure that occurs when standing up, also called orthostatic hypotension. For example, the drug fludrocortisone boosts blood volume. It's often used to treat orthostatic hypotension.
If you have long-term orthostatic hypotension, midodrine (Orvaten) may be prescribed to raise standing blood pressure levels. This medicine lessens the ability of the blood vessels to expand, which raises blood pressure.Complications/side effects of the treatment
The complications of treatment depend on the exact medication or treatment you receive. Your healthcare provider can best explain the possible complications or side effects. That’s because they can consider your specific circumstances, including other health conditions, medications you take and more.
How soon after treatment will I feel better?
Depending on the cause of your hypotension, you may feel better as you receive treatment. In some cases, it may take longer — days or even weeks — for medication or other treatments to help you feel better consistently.
Prevention
How can I lower my risk of low blood pressure?
It’s usually not possible to reduce your risk of or prevent hypotension. The only exception is avoiding circumstances or actions that can lead to it, such as taking recreational drugs or supplements/herbal remedies that can lower your blood pressure.
Eating smaller meals with fewer carbohydrates may help you avoid having low blood pressure after meals.
Your provider may recommend certain steps to prevent or reduce your symptoms including:
- Drinking more fluids
- Getting up slowly after sitting or lying down
- Not drinking alcohol
- Not standing for a long time (if you have NMH)
- Using compression stockings so blood does not collect in the legs
Prognosis
What can I expect if I have low blood pressure?
If you have hypotension, what you can expect depends on what causes it and if you have symptoms. If you don’t have symptoms, it’s unlikely that hypotension will be a problem for you.
If you have symptoms, hypotension can interfere with your ability to stand up, care for yourself, cook, drive and do many other activities. That’s why understanding low blood pressure and following a healthcare provider’s guidance are so important to minimizing this condition’s impact on your life.
How long low blood pressure lasts
How long this condition lasts depends on what caused it. If you have hypotension because of normal aging, it’ll probably be a lifelong concern.
Outlook for low blood pressure
If you have low blood pressure but don’t have symptoms, this condition usually isn’t harmful and shouldn’t impact your life.
If you do have symptoms, the underlying cause is usually what determines the outlook for this condition. Your healthcare provider is the best person to tell you what to expect from this condition and what you can do to manage those effects.
Living With
How do I take care of myself?
If you have hypotension with symptoms, the best thing you can do is follow your healthcare provider’s guidance on managing this condition. Their recommendations may include any of the following:
- Drink more water, less alcohol. Alcohol is dehydrating and can lower blood pressure, even in moderation. Water boosts the amount of blood in the body and prevents dehydration..
- Pay attention to body positions. Gently move from lying flat or squatting to a standing position. Don't sit with legs crossed.
If symptoms of low blood pressure begin while standing, cross the thighs like a pair of scissors and squeeze. Or put one foot on a ledge or chair and lean as far forward as you can. These moves encourage blood flow from the legs to the heart.- Eat small, low-carb meals. To help prevent blood pressure from dropping sharply after meals, eat small meals several times a day. Limit high-carbohydrate foods such as potatoes, rice, pasta and bread.
A healthcare professional also might recommend drinking one or two strong cups of caffeinated coffee or tea with breakfast. Caffeine can cause dehydration, though, so be sure to drink plenty of water and other fluids without caffeine.- Exercise regularly. As a general goal, work up to at least 150 minutes of moderate aerobic exercise a week. For example, you could aim to get about 30 minutes of activity most days. Also, aim to do strength-training exercises at least twice a week. But try not to exercise in hot, humid conditions.
- Having a seat: If you notice yourself feeling dizzy or lightheaded, sit down. Falling from a standing height can put you at risk for severe or even catastrophic injuries, such as a broken hip, concussion, skull fracture or broken ribs.
When should I see my healthcare provider?
If you know you have hypotension, you should see your healthcare provider if you start to notice symptoms affecting your life or disrupting your usual routine and activities.
If you don’t know you have hypotension, you should see a healthcare provider if you have repeated dizziness or fainting episodes. This is especially important because those symptoms are possible with many other health conditions, some of which are dangerous.
Call your doctor if:
- You have any of the symptoms listed above.
- You've been diagnosed with low blood pressure and are more often having symptoms, such as falling down or passing out.
- You have symptoms as a result of taking prescription or nonprescription medication.
When should I go to the ER?
If you have hypotension, you should go to the hospital when you:
- Have chest pain.
- Pass out or faint.
- Fall because of lightheadedness and hit your head (especially if you’re taking any blood-thinning medications). You should also go to the hospital if you injure yourself because of a fall from passing out.
- Have any symptoms of shock, such as feeling cold, being sweaty, breathing fast or having a fast heart rate. You may also have a blue tint to the skin of your lips or under your fingernails.
What questions should I ask my doctor?
For low blood pressure, basic questions to ask your healthcare professional include:
- What is likely causing my symptoms or condition?
- What are other possible causes?
- What tests will I need?
- What's the most appropriate treatment?
- How often should I be screened for low blood pressure?
- I have other health conditions. How can I best manage them together?
- Are there restrictions I need to follow?
- Should I see a specialist?
- Are there brochures or other printed materials I can have? What websites do you recommend?
What to expect from your doctor
Your healthcare professional is likely to ask you questions, including:
- Do you always have symptoms of low blood pressure, or do they come and go?
- How severe are your symptoms?
- What, if anything, seems to improve your symptoms?
- What, if anything, appears to make your symptoms worse?
- Do you have a family history of heart disease?
One Final Note..
Hypotension is a condition that can have no symptoms, and many people don’t even know they have it. For others, it can cause symptoms that are unpleasant and even disruptive to your daily life and activities. If you suspect you have low blood pressure, getting it diagnosed and treated is essential. A proper diagnosis and treatment can help you avoid falls and other complications. Fortunately, this condition is often treatable, and there are many things your healthcare provider can explain to you that can help you care for yourself. See your doctor if you have low blood pressure symptoms.
Find me on Social Media
 |
Don't forget to bookmark me to see updates.. Copyright © 2000 - 2025 K.
Kerr |







