- Main Page
- A1C Test
- Advance Directives
- Age on other Planets
- Aliens
- American Flag
- Annuals
- Anxiety
- Aortic Aneurysm
- Apple Cider Vinegar
- Arrhythmia
- Atrial Fibrillation
- Avoiding Scams
- Awareness Ribbons
- Bamboo
- Banana Tree, Grand Nain
- Banana Tree, Ice Cream
- Banana Tree, Zebrina Rojo
- Beekeeping
- Benign P P Vertigo
- Birth Month
- Blood Tests
- Blood Types
- Body Mass Index - BMI
- BMI Calculator
- Boogaloo
- Bookmarks
- Boot Anatomy
- Boot Fit Guide
- Boot Glossary
- Boot Leathers
- Boot Makers
- Boot Retailers
- Boot Styles - Western
- Boot Toes & Heels - Western
- Boot Toes & Heels - Work
- Bronchitis
- Candle Colors
- Carbohydrates
- Cardiac Catheterization
- Cardiovascular Disease
- CGM's
- Chakras
- Chinese Zodiac
- Cholesterol
- Christmas Tree
- Color Codes Chart
- C.O.P.D.
- Coronary Artery Disease
- Country Stars
- Cowboy Hat Etiquette
- Cowboy Hat Sizing
- C.P.A.P.
- Credit Score Checkers
- Crystals & Gems
- CT scan
- Degenerative Disk Disease
- Depression
- Diabetes Info.
- Diabetes Facts
- Diabetes - Pre
- Diabetes - Type 1
- Diabetes - Type 2
- Diabetes - Type 3c
- Diabetes - Gestational
- Diabetes Care
- Diabetes Care Team
- Diabetes Terms
- Diabetes Treatment
- Diabetes & Fruits
- Diabetes & Veg's
- Diet - Boiled Egg
- Diet - DASH
- Diet - Fat Burning
- Diet - Mediterranean
- Diet - Military
- Disability
- Do Not Resuscitate
- Dream Catchers
- Dupixent®
- Echocardiogram
- Electrocardiogram
- Emphysema
- Epsom Salt
- Eye Teasers
- Fairies
- Farxiga®
- Flower Astrology
- Fonts
- Foods To Regrow
- Friend
- Funny Things
- Fun Stuff
- Glycemic Index
- Gout
- Growing Blueberries
- Halloween
- Halloween Treats
- Headaches
- Health Info. Lines
- Heart Attack
- Heart Disease - Other
- Heart Failure
- Heart Tests
- Hello!!
- Herbal Codes
- Herbal Medicine
- Herb & Oils Uses
- Herniated disk
- Home Remedies
- House Plants
- Humalog®
- Hydrogen Peroxide
- Hyperglycemia
- Hypoglycemia
- Hyperkalemia
- Hypokalemia
- Hypertension
- Hypotension
- Important Numbers
- Insomnia
- Insulin
- Juice Recipes
- Karma
- Kidney Cysts
- Kidney Disease
- Kinds of Tea
- Lantus®
- Lemon Cleanse
- Logger vs Lineman
- Macaroni!!
- Medicare
- Mental Health
- MO HealthNet
- Moon Phases
- Mounjaro®
- MRI Scan
- My Athletic Shoes
- My Boots & Spurs
- My Cowboy Hats
- Myelography
- Mystical Unicorn
- Nasal Polyps
- Natal Astrology Chart
- Never Forget
- Nuclear Medicine
- Nutrition - Adults
- Nutrition - Adults, Older
- Nutrition - Kids
- Obesity
- One Little Rose
- Orchid Growing
- Orchid Sources
- Pagan Humor
- Pagans vs.Wiccans
- Parking Spaces
- PayPal.Me
- Pentagram vs. Pentacle
- Perennials
- Peripheral Artery Disease
- PET/CT Scan
- PET Scan
- Phobias A-Z
- Plant Care
- Plant Zone Map
- Potassium
- Propagating Plants
- Prurigo Nodularis
- Psychic Gifts
- PVC's
- Quit Smoking
- Recipes I like
- Red Yeast Rice
- Roses
- Runes
- Sadie & Beethoven
- Salt & Sodium
- Salt Water Flush
- Sciatica
- Service Animals
- Shape Shifters
- Sleep Apnea
- Sleep Disorders
- Sleep Studies
- Smile
- SPECT Scan
- Speed Test
- Spices You Need
- Spices I Have
- Spinal Stenosis
- Stents
- Steel Toe vs. Comp. Toe
- Stress Test - Exercise
- Stress Test - Nuclear
- Sugars - Sweeteners
- Superstitions
- Symbols
- Tarot
- The Ten Commandments
- Tools of the Craft
- Top Expensive Movies
- Top Modern Westerns
- Top 100 Westerns
- Toyota Yaris 2008
- Toyota Yaris 2012
- Trazodone
- Tree, Calamondin Orange
- Tree, Lemon (Meyer)
- Tree, Lime
- Tree Signs
- Ultrasound
- US Bill of Rights
- US Constitution
- US Declaration of Independence
- Vaccines by Age
- Vaccines 0-6 yrs
- Vaccines 7-18 yrs
- Vaccines 19 and up
- Ventricular Fibrillation
- Vertigo
- Vital Records
- Vital Signs
- Vitamin B12
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin K
- Vitamins & Minerals
- Water Therapy
- Weight on other Planets
- Wiccan Rede
- X-Rays
- Yin / Yang
- Zodiac Signs
Needed to read PDF's
Cardiac Catheterization
What Is Cardiac Catheterization?
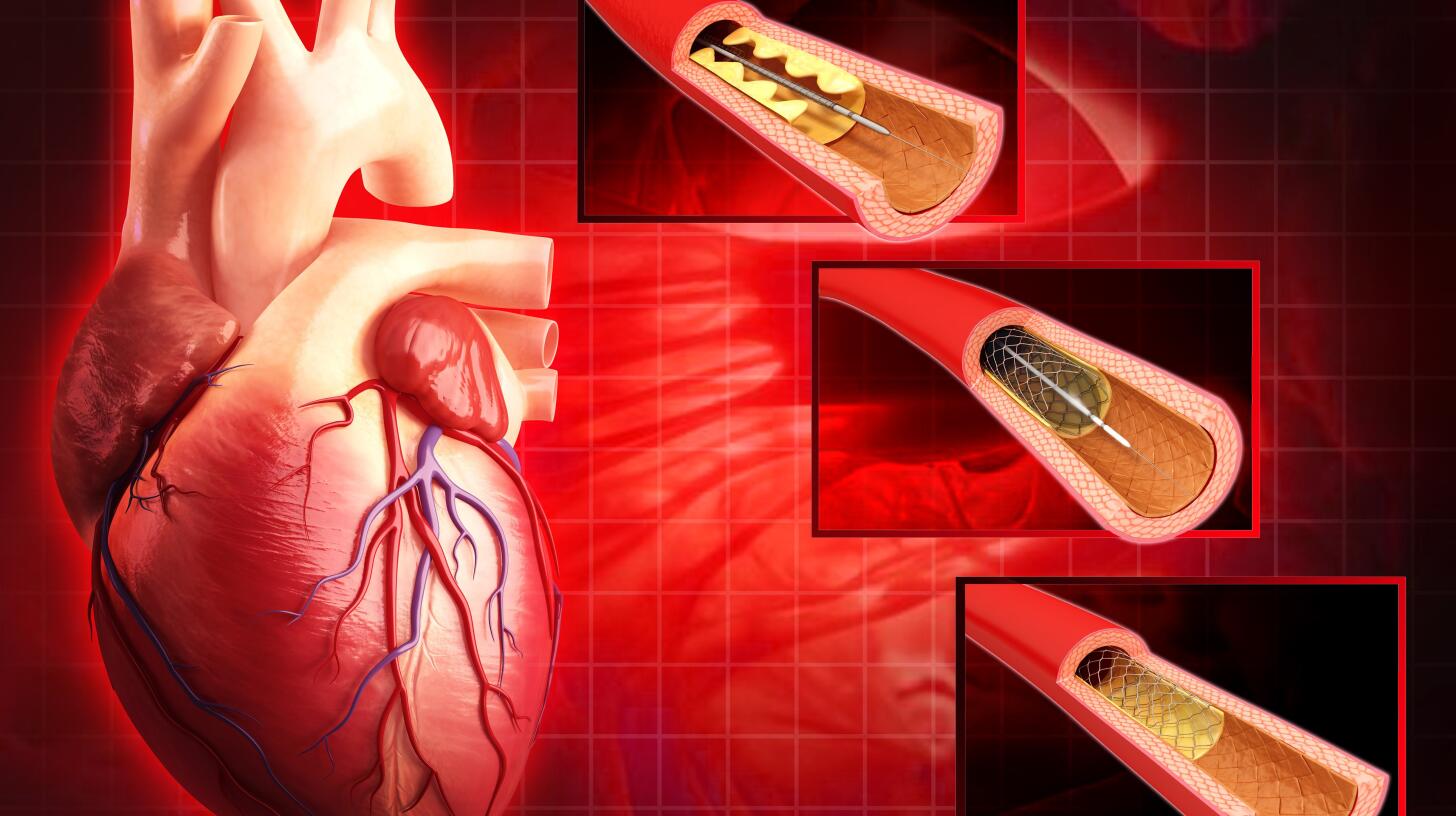
Cardiac catheterization, also known as cardiac cath or heart catheterization, is a medical procedure used to diagnose and treat some heart conditions. It lets doctors take a close look at the heart to identify problems and to perform other tests or procedures.
Your healthcare provider may recommend cardiac catheterization to find out the cause of symptoms such as chest pain or irregular heartbeat. Before the procedure, you may need to diagnostic tests, such as blood tests, heart imaging tests, or a stress test, to determine how well your heart is working and to help guide the procedure.
During cardiac catheterization, a long, thin, flexible tube called a catheter is put into a blood vessel in your arm, groin or upper thigh, or neck. The catheter is then threaded through the blood vessels to your heart. It may be used to examine your heart valves or take samples of blood or heart muscle. Your doctor may also use ultrasound, a test that uses sound waves to create an image, or they may inject a dye into your coronary arteries to see whether your arteries are narrowed or blocked. Cardiac catheterization may also be used instead of some heart surgeries to repair heart defects and replace heart valves.
Cardiac catheterization is safe for most people. Problems following the procedure are rare but can include bleeding and blood clots. Your healthcare provider will monitor your condition and may recommend medicines to prevent blood clots.
Who Needs a cardiac catheterization?
Your healthcare provider may recommend cardiac catheterization to find out what is causing symptoms of a heart problem or to treat or repair a heart problem.
Cardiac catheterization can be used for different purposes.
- Give a better understanding of other test results, such as echocardiography (echo), cardiac MRI, and cardiac CT scan. This is especially helpful if the results from those tests could not identify the problem or differ from what your doctor finds when examining you.
- Diagnose heart conditions such as arrhythmia, heart attack, pulmonary hypertension, cardiomyopathy, coronary heart disease, and heart valve diseases, including aortic stenosis and mitral regurgitation.
- Evaluate you before a possible heart surgery, such as a heart transplant.
- Measure oxygen levels and blood pressure in the chambers of your heart and the pulmonary arteries.
Your doctor may do other procedures to diagnose or treat your condition during cardiac catheterization.
- Collect biopsies of small samples of heart tissue for more laboratory testing. Biopsies can be used for genetic testing, to check for myocarditis (a type of heart inflammation), or to look for transplant rejection.
- Use coronary angiography to look at the heart or blood vessels by injecting dye through the catheter.
- Perform minor heart surgery to treat congenital heart defects and replace or widen narrowed heart valves.
- Use percutaneous coronary intervention (PCI) to open narrowed or blocked areas of the coronary arteries. PCI may include balloon dilation, also known as angioplasty , or stent placement. Most people who have heart attacks or underlying heart disease have narrowed or blocked coronary arteries.
- Apply catheter ablation to treat arrythmias.
Who should not have cardiac catheterization?
Your doctor may wait to do the procedure or recommend that you do not have cardiac catheterization if you have any of the following conditions:
- Abnormal electrolyte levels in your blood
- Acute gastrointestinal bleeding
- Acute kidney failure, or serious kidney disease that is not being treated with dialysis
- Acute stroke
- Blood that is too thin from blood-thinning medicines or other causes
- High levels of digoxin, a heart medicine used to treat heart failure or arrhythmia, in your blood
- Previous serious allergic reaction to the dye that is used during cardiac catheterization
- Severe anemia, which is a lower-than-normal amount of red blood cells or hemoglobin
- Unexplained fever
- Untreated infection
Preparing for a Cardiac Catheterization
Before cardiac catheterization, you will meet with your cardiologist, a doctor who specializes in the heart. You will be asked about your medical history, including what medicines you are taking and any allergies you may have, and you will have a physical exam. You will also get instructions on how to prepare for the procedure.
Diagnostic tests and procedures
You may need to have some tests before your catheterization procedure.
- An electrocardiogram (ECG or EKG) looks at your heart’s rhythm and other electrical activity. It can show arrhythmias, heart attacks, and other heart problems.
- A chest X-ray looks at your lungs, your heart, your major blood vessels, and other structures in your chest.
- An echocardiogram (echo) looks at the structure and function of your heart.
- A stress test looks at how well your heart works during physical stress. The stress may be physical exercise, such as walking on a treadmill, or it may be caused by a medicine that can be given to get the same effect.
- A Cardiac CT (computed tomography) scan looks for narrowing of your heart’s blood vessels and problems with the heart, larger blood vessels, and heart valves. These pictures may also help your doctor plan for procedures to open the coronary arteries.
- Cardiac MRI (magnetic resonance imaging) provides information on the structure and function of your heart, as well as the type and severity of heart disease.
- Blood tests check for certain diseases and conditions. A complete blood count (CBC) checks your hemoglobin and platelet levels. Blood chemistry tests check how well your liver and kidneys are working. Other tests may check your blood’s ability to clot.
Preparing for the procedure
Talk to your healthcare providers about your medical history, including medicines you take, other surgical procedures you’ve had, and any medical conditions you have, such as diabetes or kidney disease.
Your healthcare provider will talk to you about how to prepare for the procedure, including:
- When to arrive at the hospital and where to go.
- When you should stop eating or drinking.
- If and when you should start or stop taking medicines.
- How long you should expect to stay.
- What happens during the procedure.
- What to expect after the procedure, including potential problems, such as bleeding or soreness.
- Instructions for recovering after the procedure, including what medicines to take.
How does cardiac catheterization work?
A provider uses contrast material to outline your vessels and heart chambers in images. They create X-ray movies (coronary angiogram) as the contrast material moves through your heart.
Digital photos of the contrast material allow your provider to:
- Identify the site of the narrowing or blockage in a coronary artery
- Evaluate the size and shape of heart chambers and blood vessels
- Find abnormal leaks or holes
In some cases, your healthcare provider may want to get better detail by using other imaging procedures during your cardiac cath.
These may include:
- Intravascular ultrasound (IVUS) to see plaque and calcium buildup or check stent placement
- Fractional flow reserve (FFR) to measure the pressure on both sides of a blockage and see if a blockage is bad enough to need treatment
- Optical coherence tomography (OCT) to take pictures inside blood vessels
Your provider may also want to perform procedures during your cardiac cath.
These nonsurgical treatments may include:
- Angioplasty to open narrowed coronary arteries and improve blood flow to your heart
- Stent placement to help an opened artery stay that way
- Valvuloplasty to open a narrow heart valve
- Rotablation to treat calcium deposits in arteries
- Intravascular lithotripsy to break up calcium with pressure waves and a special balloon
- Cardiac ablation to correct an abnormal heart rhythm
During Cardiac Catheterization
Cardiac catheterization takes place in a catheterization laboratory, or cath lab, which is similar to a small operating room. The procedure is often done in a hospital, but you may be able to have the procedure in a catheterization lab located in a medical clinic, depending on the reason for the procedure.
What happens next depends on why you're having the procedure. These are some common reasons:
- Coronary angiogram. This test checks for blockages in the arteries leading to the heart. The catheter is placed in a blood vessel, usually in the groin or wrist. Dye flows through the catheter. Then X-ray images of the heart arteries are taken. The dye helps blood vessels show up more clearly on the X-ray images.
- Cardiac ablation. Heat or cold energy is used to create tiny scars in the heart to block irregular electrical signals. This procedure is used to correct heart rhythm problems.
- Right heart catheterization. This is done to check the pressure and blood flow in the right side of the heart. A catheter is inserted in a vein in the neck or groin. The catheter has special sensors in it.
- Balloon angioplasty, with or without stenting. This treatment uses a catheter and a tiny balloon to open a narrowed artery in or near the heart. The catheter is inserted in either the wrist or groin. A mesh tube called a stent is sometimes placed in the artery to keep it open.
- Balloon valvuloplasty. This treatment uses a catheter and a tiny balloon to widen a narrowed heart valve. The placement of the catheter depends on the specific type of heart valve problem.
- Heart valve replacement. Doctors can use a catheter to remove a narrowed heart valve and replace it with an artificial valve. An example is transcatheter aortic valve replacement (TAVR).
- Repair a heart problem you're born with, also called a congenital heart defect. Cardiac catheterization methods may be used to close holes in the heart, such as an atrial septal defect or patent foramen ovale.
- Heart biopsy. Sometimes a sample of heart tissue needs to be taken to examine under a microscope. During a heart biopsy, the catheter is usually placed in the vein in the neck. Less often, it may be placed in the groin. A catheter with a small, jaw-like tip is used to obtain a small piece of tissue from the heart.
How is cardiac catheterization done?
During your cardiac catheterization procedure, a healthcare provider will:
- Inject a numbing medicine under your skin with a small needle
- Insert a plastic introducer sheath (a short, hollow tube the catheter goes through) in a blood vessel in your arm, neck or groin
- Insert a catheter through the sheath and thread it to your heart (you may feel pressure when your provider puts in the introducer sheath or catheter, but you shouldn’t feel pain)
- Ask you to turn your head or take a deep breath and hold it for a few seconds to help position the catheter
- Dim the lights and inject a small amount of contrast material through the catheters into your arteries and heart chambers. You may feel hot or flushed for several seconds
- Use an X-ray camera to take photographs of your arteries and heart chambers while the contrast is flowing through them (you may need to hold your breath while your provider takes the X-rays)
- Remove the catheter and sheath while you stay still
- Turn the lights on
Types of cardiac catheterization
The two types of cardiac catheterization are:
- Left heart catheterization. Working through an artery, this type looks at your coronary arteries and heart chambers and measures pressures on the left side of your heart.
- Right heart catheterization. Working through a vein, this type looks at your heart chambers and measures pressures on the right side of your heart.
Why a heart catheterization procedure?
Cardiac catheterization is used to:
- Find out why you’re having chest pain or an abnormal heart rhythm
- Take blood or a tiny bit of muscle from your heart to examine (biopsy)
- Confirm that you have issues in your coronary arteries or heart valves
- Evaluate heart muscle function and diagnose heart muscle disease (cardiomyopathy)
- Check your pulmonary arteries for issues and diagnose high blood pressure in those arteries (pulmonary hypertension)
- Check on your blood flow, oxygen level and pressure in areas of your heart
- Get more information that other tests couldn’t provide
- Decide on further treatment, like clearing a blockage, placing a stent or bypassing a blockage with coronary artery bypass graft (CABG)
- Help with planning a heart transplant
Possible risks
Cardiac catheterization is a relatively safe procedure, and complications are rare. However, as with any procedure involving the heart and blood vessels, there are some risks.
Possible risks include the following:
- Allergic reaction to the dye
- Irregular heart rhythm (arrhythmia)
- Bleeding or discomfort where the catheter was inserted
- Blood clots
- Collapsed lung, called pneumothorax
- Damage to blood vessels, heart valves, or the heart from the catheter
- Heart attack
- Hypothermia, or very low body temperature, especially for small children
- Infection
- Low blood pressure from bleeding or as a reaction to the procedure
- Need for a blood transfusion
- Need for emergency surgery to repair a tear in a blood vessel, such as the aorta or a coronary artery, and restore blood flow to the heart. This may be done using a coronary artery bypass graft (CABG).
- Side effects of the medicine to help you relax or sleep, if used. These can include nausea, vomiting, confusion, or an allergic reaction.
- Side effects of radiation. Although not an immediate risk, repeated radiation exposure from X-rays used to place the catheter may increase the risk of cancer and leukemia, skin damage, and cataracts later in life. This is especially true for children.
- Stroke
When you talk with your provider, ask questions to make sure you understand all of the potential risks and why they recommend the procedure.
Although cardiac catheterization isn’t surgery, you may consider it a serious procedure. But people rarely have complications from a heart cath. Providers perform more than one million cardiac catheterizations in the U.S. each year.
What happens after the procedure?
Your healthcare provider will remove the catheters and sheath after your procedure.
If you had a catheter in your arm for your cardiac cath, you can expect to:
- Have a bandage on the puncture site
- Keep your arm straight for at least an hour (but you’ll be able to walk around)
- Be under observation for a few hours to monitor any symptoms or side effects of the procedure
- Get instructions on how to care for your arm when you go home
- Tell your provider if you think you’re bleeding (wet, warm sensation) or feeling any numbness or tingling in your fingers
If you had a catheter at your groin for your heart cath, your provider will:
- Close your puncture site with applied pressure, and sometimes a suture device or a “plug” that works with your body to form a clot (this reduces the risk of bleeding)
- Ask you to lie flat and keep your leg straight for two to six hours to prevent bleeding (less time if they used a plug) — they’ll also ask you not to raise your head more than two pillows high
- Place a sterile dressing on your groin area to protect it from infection and check it regularly
- Ask you to let them know if you think you’re bleeding (have a wet, warm sensation) or if your toes begin to tingle or feel numb
Recovering from a Cardiac Catheterization
For heart catheterization recovery, you’ll:
- Need to drink plenty of liquids to clear the contrast material from your body
- Find out from your provider if you’ll be going home or staying overnight (in either case, they’ll monitor you for several hours after the procedure)
- Talk with your provider about caring for your wound site
- Need to have a friend or family member drive you home (you should stay in a hotel if you have more than a two-hour drive home, and stop every hour and walk for five to 10 minutes)
You can usually drive 24 hours after leaving the hospital. Depending on where the catheter was, you’ll need to avoid strenuous activities (including sports and lifting) for two to five days. Your healthcare provider can tell you when you can return to work.
During your recovery at home, you shouldn’t submerge the puncture site in water for a week. That means no swimming or taking baths. But you may shower 24 hours after the procedure.
Receive follow-up care
What type of results do you get and what do the results mean?
After completing your cardiac catheterization, your healthcare provider will have a lot of information they can use to decide your next step in treatment. Depending on the reason for your heart catheterization, your results can vary.
Your provider may:
- Find and fix a problem like a blockage in your coronary artery
- Diagnose you with a condition that requires surgery
- Send a tissue sample of your heart muscle to the lab for a biopsy
- Get the information they need to plan treatment
- Find that your heart is working well after a previous treatment
When should I know the results of the test?
Your healthcare provider may discuss your results with you right away. For something that takes more time, like a lab analysis of a tissue sample, it might take a few days to get results.
If the results are abnormal, what are the next steps?
If your healthcare provider found a problem during the heart cath, they may schedule another procedure. With the information they gathered, they may start planning for a surgery.
When to call the doctor
Late complications from cardiac catheterization are rare but can be serious. A small bruise and tenderness at the access site is normal. Call your healthcare provider immediately if you experience any of the following, as they may be signs of serious problems:
- Bleeding from the access site that cannot be stopped with firm pressure
- Chest pain or shortness of breath
- Dizziness
- Fever
- Increased pain, redness, or bruising at the access site
- Irregular, very slow, or fast heartbeat
- Swelling at the access site
- Yellow or green discharge draining from the access site
- Your leg or arm that was used for access becoming numb or weak, or any part of it turning cold or blue
Other serious complications after catheterization, although rare, include heart attack and stroke. Know the signs of a heart attack and signs of a stroke, and call 9-1-1 immediately if you or someone else is having symptoms.
One Final Note..
It can be scary to think about someone looking at your heart from the inside. But a cardiac catheterization isn’t surgery and your team will keep you comfortable. A heart cath provides valuable information your healthcare provider can use to decide their next steps. Collecting that information gets you one step closer to a treatment that’s best for you. Don’t hesitate to ask your provider any questions you have.
Find me on Social Media
 |
Don't forget to bookmark me to see updates.. Copyright © 2000 - 2025 K.
Kerr |







