- Main Page
- A1C Test
- Advance Directives
- Age on other Planets
- Aliens
- American Flag
- Annuals
- Anxiety
- Aortic Aneurysm
- Apple Cider Vinegar
- Arrhythmia
- Atrial Fibrillation
- Avoiding Scams
- Awareness Ribbons
- Bamboo
- Banana Tree, Grand Nain
- Banana Tree, Ice Cream
- Banana Tree, Zebrina Rojo
- Beekeeping
- Benign P P Vertigo
- Birth Month
- Blood Tests
- Blood Types
- Body Mass Index - BMI
- BMI Calculator
- Boogaloo
- Bookmarks
- Boot Anatomy
- Boot Fit Guide
- Boot Glossary
- Boot Leathers
- Boot Makers
- Boot Retailers
- Boot Styles - Western
- Boot Toes & Heels - Western
- Boot Toes & Heels - Work
- Bronchitis
- Candle Colors
- Carbohydrates
- Cardiac Catheterization
- Cardiovascular Disease
- CGM's
- Chakras
- Chinese Zodiac
- Cholesterol
- Christmas Tree
- Color Codes Chart
- C.O.P.D.
- Coronary Artery Disease
- Country Stars
- Cowboy Hat Etiquette
- Cowboy Hat Sizing
- C.P.A.P.
- Credit Score Checkers
- Crystals & Gems
- CT scan
- Degenerative Disk Disease
- Depression
- Diabetes Info.
- Diabetes Facts
- Diabetes - Pre
- Diabetes - Type 1
- Diabetes - Type 2
- Diabetes - Type 3c
- Diabetes - Gestational
- Diabetes Care
- Diabetes Care Team
- Diabetes Terms
- Diabetes Treatment
- Diabetes & Fruits
- Diabetes & Veg's
- Diet - Boiled Egg
- Diet - DASH
- Diet - Fat Burning
- Diet - Mediterranean
- Diet - Military
- Disability
- Do Not Resuscitate
- Dream Catchers
- Dupixent®
- Echocardiogram
- Electrocardiogram
- Emphysema
- Epsom Salt
- Eye Teasers
- Fairies
- Farxiga®
- Flower Astrology
- Fonts
- Foods To Regrow
- Friend
- Funny Things
- Fun Stuff
- Glycemic Index
- Gout
- Growing Blueberries
- Halloween
- Halloween Treats
- Headaches
- Health Info. Lines
- Heart Attack
- Heart Disease - Other
- Heart Failure
- Heart Tests
- Hello!!
- Herbal Codes
- Herbal Medicine
- Herb & Oils Uses
- Herniated disk
- Home Remedies
- House Plants
- Humalog®
- Hydrogen Peroxide
- Hyperglycemia
- Hypoglycemia
- Hyperkalemia
- Hypokalemia
- Hypertension
- Hypotension
- Important Numbers
- Insomnia
- Insulin
- Juice Recipes
- Karma
- Kidney Cysts
- Kidney Disease
- Kinds of Tea
- Lantus®
- Lemon Cleanse
- Logger vs Lineman
- Macaroni!!
- Medicare
- Mental Health
- MO HealthNet
- Moon Phases
- Mounjaro®
- MRI Scan
- My Athletic Shoes
- My Boots & Spurs
- My Cowboy Hats
- Myelography
- Mystical Unicorn
- Nasal Polyps
- Natal Astrology Chart
- Never Forget
- Nuclear Medicine
- Nutrition - Adults
- Nutrition - Adults, Older
- Nutrition - Kids
- Obesity
- One Little Rose
- Orchid Growing
- Orchid Sources
- Pagan Humor
- Pagans vs.Wiccans
- Parking Spaces
- PayPal.Me
- Pentagram vs. Pentacle
- Perennials
- Peripheral Artery Disease
- PET/CT Scan
- PET Scan
- Phobias A-Z
- Plant Care
- Plant Zone Map
- Potassium
- Propagating Plants
- Prurigo Nodularis
- Psychic Gifts
- PVC's
- Quit Smoking
- Recipes I like
- Red Yeast Rice
- Roses
- Runes
- Sadie & Beethoven
- Salt & Sodium
- Salt Water Flush
- Sciatica
- Service Animals
- Shape Shifters
- Sleep Apnea
- Sleep Disorders
- Sleep Studies
- Smile
- SPECT Scan
- Speed Test
- Spices You Need
- Spices I Have
- Spinal Stenosis
- Stents
- Steel Toe vs. Comp. Toe
- Stress Test - Exercise
- Stress Test - Nuclear
- Sugars - Sweeteners
- Superstitions
- Symbols
- Tarot
- The Ten Commandments
- Tools of the Craft
- Top Expensive Movies
- Top Modern Westerns
- Top 100 Westerns
- Toyota Yaris 2008
- Toyota Yaris 2012
- Trazodone
- Tree, Calamondin Orange
- Tree, Lemon (Meyer)
- Tree, Lime
- Tree Signs
- Ultrasound
- US Bill of Rights
- US Constitution
- US Declaration of Independence
- Vaccines by Age
- Vaccines 0-6 yrs
- Vaccines 7-18 yrs
- Vaccines 19 and up
- Ventricular Fibrillation
- Vertigo
- Vital Records
- Vital Signs
- Vitamin B12
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin K
- Vitamins & Minerals
- Water Therapy
- Weight on other Planets
- Wiccan Rede
- X-Rays
- Yin / Yang
- Zodiac Signs
Needed to read PDF's
Atrial Fibrillation
(Afib)
Atrial fibrillation (Afib) is an irregular heart rhythm that begins in your heart’s upper chambers (atria). Symptoms include fatigue, heart palpitations, trouble breathing and dizziness. Afib is one of the most common arrhythmias. Risk factors include high blood pressure, coronary artery disease and having obesity. Untreated Afib can lead to blood clots, stroke and heart failure. Five million Americans are estimated to be living with AFib today, and more than 12 million people are projected to have it by 2030.
Overview
What is Afib?
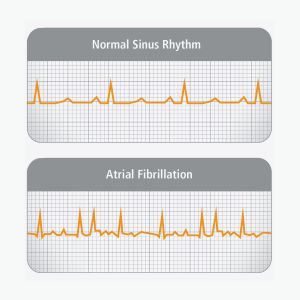
Atrial fibrillation is an irregular heartbeat, or arrhythmia. Atrial fibrillation, also known as AFib or AF, can lead to blood clots, stroke, heart failure and other heart-related complications. AFib is the most common type of irregular heart rhythm. With Afib, your heart’s electrical system doesn’t work as it should. Instead of a steady, regular pattern of electrical impulses firing, many different impulses fire rapidly at the same time.
This causes a fast, chaotic rhythm in your atria instead of a regular rhythm and pace. As a result, your atria can’t do a good job of contracting or pumping blood into your lower chambers (ventricles). Your ventricles, which respond to your atria, also contract irregularly, causing a rapid, irregular heartbeat. (The heartbeat and pulse that you feel come from your ventricles’ contractions.) Your ventricles may get 140 to 160 signals per minute instead of the normal 60 to 100 per minute.
You can think of Afib like several conductors directing an orchestra instead of just one. The musicians wouldn’t know who to follow or what to do. The music would lose its rhythm.
Atrial fibrillation can lead to a stroke and other serious medical issues like heart failure. That’s why it’s important to learn the symptoms and talk with your healthcare provider about your personal risk factors.
Fortunately, there are many ways to bring back your heart’s rhythm if you have Afib. It all starts with a visit to your healthcare provider, who can run some tests and make a diagnosis.
Types of Afib
Providers classify atrial fibrillation based on how long the Afib episodes last.
- Paroxysmal Afib episodes last less than one week and usually go away on their own without treatment. People can still feel unwell during these short periods of Afib, and people with paroxysmal Afib still have a higher risk of stroke than those without Afib at all. Paroxysmal Afib can progress to persistent Afib depending on your risk factors.
- Persistent Afib episodes last more than one week and generally need specialized treatment to either slow the heart rate down or break the Afib back to normal sinus rhythm.
- Long-term persistent Afib lasts more than a year and can be difficult to treat.
- Permanent Afib describes long-term Afib that hasn’t been responsive to attempts at breaking and staying out of Afib.
What happens during AFib?
Normally, your heart contracts and relaxes to a regular beat. In AFib, the upper chambers of the heart, or the atria, beat irregularly. Not enough blood is being pumped out of the atria, so blood pools there. The pooled blood can clot, which can be very dangerous.
If a blood clot forms, it can be pumped out of the heart to the brain. This blocks the blood supply to the brain and cause a stroke.
About 12% to 20% of people who have strokes caused by blood clots or attributed to large or small vessel disease have this abnormal heart rhythm. The clot risk is why people with this condition may be prescribed blood thinners*.
AFib can double the risk of death and is linked with an estimated fivefold increased risk for stroke. Yet many people are unaware that AFib is a serious condition.
Symptoms, Causes, & Risks
Symptoms of Afib
Some people have symptoms, and some don’t. It depends on how fast your ventricles are beating. If they’re beating at a normal or slightly elevated pace, you probably won’t feel anything. But if your ventricles beat faster, you’ll start to notice symptoms.
These can include:
- Extreme fatigue.
- An irregular heartbeat.
- Heart palpitations.
- A feeling of butterflies or a fish flopping in your chest.
- Dizziness or lightheadedness.
- Fainting (syncope).
- Shortness of breath (dyspnea).
- Chest pain (angina).
If you have atrial fibrillation symptoms, keep a list of when they happen and share this information with your healthcare provider right away.
What causes Afib?
Changes or damage to your heart’s tissue and electrical system cause atrial fibrillation. Usually, coronary artery disease, high blood pressure or heart failure can cause these changes. Other causes include heart valve issues, hyperthyroidism or excessive alcohol use. Sometimes, when your body is sick for other reasons (like blood loss or severe infection), the stress response from the illness can cause Afib.
Often, a prematurely triggered heartbeat (which feels like a skipped beat) causes atrial fibrillation to begin. These are more common in the conditions above. But sometimes, it’s hard to know the cause of that triggered heartbeat. For some people, there’s no identifiable cause.
What are the risk factors?
While atrial fibrillation can affect anyone, it’s more common among people of European descent. But Black people who have Afib are more likely to have serious complications like stroke or heart failure. Women receive a diagnosis more often.
Afib often runs in families. If someone in your biological family has Afib, you have a higher chance of developing it, too.
The older you get, the greater your risk for atrial fibrillation. At 65 years old, your risk especially increases. Besides increasing age, high blood pressure is a huge risk factor. High blood pressure causes 1 in 5 cases of Afib.
You also have a higher risk of developing Afib if you have any of the following conditions:
- Obesity.
- Type 2 diabetes.
- Chronic kidney disease.
- Heart failure.
- Coronary artery disease.
- Congenital heart disease.
- Lung diseases, like chronic obstructive pulmonary disease (COPD).
- Sleep apnea.
- Hyperthyroidism.
In addition, using tobacco products, recreational drugs or beverages containing alcohol can raise your risk.
While physical activity strengthens your heart, some athletes who exercise intensely for long periods of time could have a higher risk of Afib. In those rare cases, reducing the intensity of activity usually helps.
An estimated 1 in 3 people with Afib doesn’t know they have it. That’s why it’s important to know the risk factors and talk with your healthcare provider. If you’re at risk, you should have your heart and pulse checked regularly so you can catch problems early.
What are the complications of Afib?
Atrial fibrillation can cause serious medical complications. So, it’s essential to learn the warning signs and to share them with your family and friends. In many cases, you need someone else to call 911. Immediately call 911 (or your local emergency services) if you have the following symptoms or if you notice them in someone around you:
- Heart attack: While it’s not common for Afib to lead to a heart attack, it’s still important to recognize the symptoms of a heart attack. Pain, discomfort or pressure in the center of your chest or upper abdomen, a feeling of squeezing, fullness, heartburn or indigestion or pain down your left arm. Females may also have pain in their back, shoulders or jaw, nausea and vomiting, shortness of breath or excessive tiredness.
- Stroke: Sudden numbness or weakness on one side of your body, confusion, trouble speaking or understanding others, difficulty seeing in one or both of your eyes, trouble walking, dizziness or sudden headache for no reason. Learn how to recognize these symptoms in yourself or others so you can act quickly. Every minute counts.
- Bleeding in your brain, digestive system or urinary tract: Bright red blood in your vomit, stool (poop) or urine (pee), severe pain in your head or abdomen, memory loss, drastic vision changes or difficulty moving your legs or arms. Many people with Afib need to take blood-thinning medications to lower the risk of Afib-related stroke. This medication is essential. But these medications can make it more difficult for active bleeding to stop.
- Heart failure: The rapid, disorganized rhythm of Afib can make it harder for your heart to pump blood forward. As a result, blood flow becomes congested as your lungs can’t drain blood forward to your heart. This can lead to some people feeling short of breath and winded when they’re in Afib. Over time, some people may see belly bloating and leg swelling. Breathing can also be more difficult when trying to lie down to sleep.
- Cardiac arrest/fainting: In certain people, Afib can lead to lightheadedness and fainting. The heart resumes beating after most cases of fainting, and people will often recover consciousness soon after they faint. In rare cases, your heart fails to pump blood to the rest of your body after you faint, and you don’t regain consciousness. This situation is called a cardiac arrest. Cardiac arrest is unpredictable, but chest pain (angina), shortness of breath, nausea and vomiting or dizziness might happen within an hour before having a cardiac arrest. In some cases, these symptoms might not appear at all, and you could simply faint.
If you or a loved one has Afib, it’s a good idea to talk with your healthcare provider about how to get help in medical emergencies. For those who live alone or spend lots of time alone, medical alert devices may be a life-saving resource.
Diagnosis and Tests
How is Afib diagnosed?
To diagnose atrial fibrillation, your healthcare provider will first ask you some questions. They’ll ask about what you eat, your physical activity, biological family history, any symptoms you’ve noticed and risk factors.
Your provider will then give you a physical exam that includes:
- Listening to your heart rhythm with a stethoscope.
- Taking your pulse and blood pressure.
- Checking the size of your thyroid gland to look for thyroid problems.
- Looking for swelling in your feet or legs to identify heart failure.
- Listening to your lungs to detect heart failure or infection.
This exam will help your provider understand your baseline health and how your body is functioning.
What tests will be done to diagnose Afib?
In addition to the physical exam, your provider may run some tests to make an atrial fibrillation diagnosis.
These tests include:
- Electrocardiogram (EKG or ECG). This records your heart’s electrical signals so your provider can see if your heart is beating normally.
- Echocardiogram (echo). An echo (heart ultrasound) can reveal problems with blood flow and heart muscle contractions. Certain echocardiograms can also reveal blood clots in your heart. Providers can do echocardiograms from outside your body (transthoracic) or inside your esophagus (transesophageal).
- Blood tests. Sometimes, imbalances in your blood can cause Afib. Simple blood tests can show your potassium and thyroid hormone levels. They can help your provider choose the best medicines for you based on your liver and kidney function.
- Cardiac MRI (magnetic resonance imaging). Without using any radiation, this imaging test lets your provider see your heart’s structure and function. For some people, this can provide clues to problems with heart structure that predispose them to Afib.
In some cases, your provider may want to check how your heart rhythm looks in your daily life. If so, they’ll ask you to wear a Holter monitor (for one or two days) or a portable event monitor (for up to one month) to record your heart’s activity.
What are the stages of AFib?
Like many heart conditions, AFib is a progressive disease. It has four stages:
Stage 1: At risk for AFib
You have not been diagnosed with AFib and can take action to prevent it from developing. You should talk with your health care professional about detecting and treating AFib early, especially if you have AFib risk factors.
Stage 2: Pre-AFib
You have not been diagnosed with AFib, but there may be abnormal structural or electrical problems in your heart that can lead to it. Your health care professional will closely watch to see if AFib develops. You may begin treatment early to slow or stop the progression.
Stage 3: AFib
You have been diagnosed with AFib. You and your health care professional will discuss how severe your condition is and the best treatment for you. Treatment could include medications to control the heart’s rhythm or rate, surgery or managing other health conditions. You will also learn how to reduce your risk of having a stroke. Your stroke risk may change with time. Your health care team can use a risk calculator to find out your risk and guide treatment decisions.
Stage 4: Permanent AFib
You have permanent AFib that can’t be treated with medications or surgery. You can still talk with your care team about managing your other health conditions, which may lessen AFib symptoms.
It’s important to recognize the different stages of AFib. Understanding your stage can help you prevent AFib, catch it early or know how far your condition has progressed. You and your health care professional can then decide on the best treatment plan for you.
Management and Treatment
How is Afib treated?
The main goals of Afib treatment include:
- Managing your heart rate.
- Regaining a normal heart rhythm.
- Reducing your risk of having a stroke.
Based on your symptoms, your healthcare provider will likely prescribe medications first to see if they help.
Medications to manage your heart rate
Some medications for atrial fibrillation treatment may keep your ventricles from beating too fast include:
- Digoxin.
- Metoprolol.
- Carvedilol.
- Verapamil.
- Diltiazem.
Medications to manage your heart rhythm
Afib treatments that help your heart beat in a normal sinus rhythm include:
- Procainamide.
- Disopyramide.
- Flecainide.
- Propafenone.
- Sotalol.
- Dofetilide.
- Amiodarone.
Blood thinners (anticoagulant medications)
Atrial fibrillation treatments that reduce your risk of blood clots and stroke include:
- Warfarin.
- Dabigatran.
- Apixaban.
- Argatroban.
Procedures and surgeries
If medications don’t help your Afib, you may need a procedure or surgery. Many procedures can be noninvasive, and newer treatment methods and technologies are constantly developing. Talk with your provider about the best options for you.
Treatments may include:
- Electrical cardioversion electrically “resets” your heart rhythm using low-energy shocks. But it may only be a temporary solution.
- Pulmonary vein isolation ablation uses catheters to deliver energy outside and around your pulmonary veins. This is commonly called an “Afib ablation.” This procedure helps you respond better to your Afib medications. You may not even need medications long-term to keep Afib away.
- A provider may put in a permanent pacemaker if you have too slow of a heart rate. Usually, you’d only get one if you have another arrhythmia in addition to Afib.
- Left atrial appendage closure is a procedure that reduces your risk of blood clots and stroke. Providers can do this with catheters or during open-heart surgery.
- The maze procedure is a surgical Afib ablation technique that a provider might do during open-heart surgery in an attempt to keep Afib away.
Prevention
How can I lower my risk?
While you can’t get rid of all of your risk factors for Afib, you may be able to change four major ones: obesity, physical inactivity, excessive alcohol consumption and tobacco use.
Here are some tips to lower your risk:
- Eat heart-healthy foods.
- Add aerobic exercise to your routine. Try for at least 150 minutes per week. Learn the target heart rate for your age and monitor your heart rate during physical activity. Be sure to talk with your provider before starting any physical activity plan.
- Limit your alcohol consumption. If you think you may have alcohol use disorder, reach out to a provider for help.
- Quit smoking and using tobacco products. It can be hard to do this alone. With the right resources and support, you can achieve this goal and make your heart healthier.
As you lower these risk factors, you’ll also see other benefits like reduced blood pressure, lower cholesterol levels and weight loss. When it comes to heart health, each positive lifestyle change has a ripple effect. The more changes you can make, the more benefits you’ll enjoy in the long run.
Prognosis
What can I expect if I have atrial fibrillation?
Afib may keep coming back, even with treatment. As atrial fibrillation progresses, it becomes more serious and harder to treat. Medicines that helped you in the past may not help in the future. Healthcare providers can’t cure Afib, but they can manage your symptoms. Talk with your healthcare provider about the best management and treatment plan for you.
Living With Afib
How do I take care of myself?
The same habits that lower your risk of Afib help you feel better when you have it. Eating healthy foods and getting 30 minutes of physical activity five days a week helps your heart. You can break up your activity into 10-minute chunks to make it easier. Cutting out tobacco products and alcohol is good for your heart, too.
When should I see my healthcare provider?
There’s no single schedule to follow. It all depends on your symptoms and treatment plan, and whether you need follow-ups after a procedure. So, it’s important to talk with your provider and make a plan together. Make sure you go to all your scheduled appointments. Keep track of the medications you’re taking and bring a list of your medications to every visit. It’s also a good idea to keep the list in your wallet so it’s with you in emergencies.
At each visit, be sure to share any new symptoms or problems you’re having, like side effects from medication. Be sure to ask your provider before taking over-the-counter (OTC) medicines, like those for cold and flu, and nutritional supplements. Sometimes, these products can affect your heart rate or interact with your prescription medications.
What questions should I ask my healthcare provider?
Questions to consider asking your provider may include:
- How can I reduce my risk factors?
- Can you connect me with a dietitian?
- Can you recommend any local health and fitness programs?
Additional Common Questions
How can I check for Afib at home?
If you think you have Afib symptoms, it’s important to call your healthcare provider right away to discuss how you’re feeling. Your provider may ask you to check your pulse. If it feels erratic or weak, that could be a sign you’re in Afib.
But sometimes, you might not notice any changes in your pulse, especially if your Afib isn’t advanced. You may instead just feel tired or out of breath. You may not know if your symptoms are from Afib or something else. That’s why a call to your provider is essential. You can’t diagnose Afib yourself.
How common is Afib?
More than 33 million people age 55+ worldwide have an Afib diagnosis. Estimates predict that 12 million people in the U.S. will have Afib by 2030. Afib causes nearly half a million hospitalizations a year in the U.S. and leads to more and more deaths with each passing year.
One Final Note..
Atrial fibrillation is a complex heart condition that can seem scary, confusing or overwhelming. But whether you suspect you might have Afib, were recently diagnosed or have been living with it for years, you’re not alone. You’re one of the millions of people learning new strategies for managing Afib while still enjoying life. That’s why it’s important to talk with your healthcare provider and learn more about available resources and support communities.
It’s also helpful to learn about the benefits and risks of treatment options. All medications or procedures carry some risks. But when it comes to Afib, treatment is essential for supporting your heart and reducing your chances of having a stroke. Your provider will work with you to choose the best approach.
Additional Resources
Patient Assistance
- Medicare.gov, The Official US Government Site for Medicare—Includes Medicare Plan Finder, Costs for Medicare Drug Coverage, and Extra Help Program
- Medicine Assistance Tool—Telephone 1-571-350-8643—Referral to patient prescription assistance programs, sponsored by the pharmaceutical industry association (PhRMA)
- Patient Advocate Foundation—Toll-free: 1-800-532-5274—Solves insurance and healthcare access issues for patients, including providing help for the uninsured and underinsured. Matters of the Heart provides a wealth of insurance and patient assistance information specifically for those with heart disease.
- RxResource.org—Resources on prescription drug coverage and prescription assistance programs
Phone Apps
- AFibLife App (Abbott)—afib information for you, trackable data for your doctor (free version, or premium with the AFEQT quality of life survey)—Download from Google Play or Apple App Store
- Cardiogram—Download from Google Play for Android Wear or App Store for Apple Watch
- CardioVisual educational heart videos in an app designed by cardiologists—Download from Google Play or Apple App Store
- Kardia/AliveCor (requires Kardia Mobile EKG monitoring device)—Download from Google Play or Apple App Store
- Medisafe Medication Tracker (Mellanie’s favorite)—Download from Google Play or Apple App Store
- Mango Health Medication Tracker—Download from Google Play or Apple App Store
- MyAF—Download from Google Play or Apple App Store (Europe and UK only)
Find me on Social Media
 |
Don't forget to bookmark me to see updates.. Copyright © 2000 - 2025 K.
Kerr |








