- Main Page
- A1C Test
- Advance Directives
- Age on other Planets
- Aliens
- American Flag
- Annuals
- Anxiety
- Aortic Aneurysm
- Apple Cider Vinegar
- Arrhythmia
- Atrial Fibrillation
- Avoiding Scams
- Awareness Ribbons
- Bamboo
- Banana Tree, Grand Nain
- Banana Tree, Ice Cream
- Banana Tree, Zebrina Rojo
- Beekeeping
- Benign P P Vertigo
- Birth Month
- Blood Tests
- Blood Types
- Body Mass Index - BMI
- BMI Calculator
- Boogaloo
- Bookmarks
- Boot Anatomy
- Boot Fit Guide
- Boot Glossary
- Boot Leathers
- Boot Makers
- Boot Retailers
- Boot Styles - Western
- Boot Toes & Heels - Western
- Boot Toes & Heels - Work
- Bronchitis
- Candle Colors
- Carbohydrates
- Cardiac Catheterization
- Cardiovascular Disease
- CGM's
- Chakras
- Chinese Zodiac
- Cholesterol
- Christmas Tree
- Color Codes Chart
- C.O.P.D.
- Coronary Artery Disease
- Country Stars
- Cowboy Hat Etiquette
- Cowboy Hat Sizing
- C.P.A.P.
- Credit Score Checkers
- Crystals & Gems
- CT scan
- Degenerative Disk Disease
- Depression
- Diabetes Info.
- Diabetes Facts
- Diabetes - Pre
- Diabetes - Type 1
- Diabetes - Type 2
- Diabetes - Type 3c
- Diabetes - Gestational
- Diabetes Care
- Diabetes Care Team
- Diabetes Terms
- Diabetes Treatment
- Diabetes & Fruits
- Diabetes & Veg's
- Diet - Boiled Egg
- Diet - DASH
- Diet - Fat Burning
- Diet - Mediterranean
- Diet - Military
- Disability
- Do Not Resuscitate
- Dream Catchers
- Dupixent®
- Echocardiogram
- Electrocardiogram
- Emphysema
- Epsom Salt
- Eye Teasers
- Fairies
- Farxiga®
- Flower Astrology
- Fonts
- Foods To Regrow
- Friend
- Funny Things
- Fun Stuff
- Glycemic Index
- Gout
- Growing Blueberries
- Halloween
- Halloween Treats
- Headaches
- Health Info. Lines
- Heart Attack
- Heart Disease - Other
- Heart Failure
- Heart Tests
- Hello!!
- Herbal Codes
- Herbal Medicine
- Herb & Oils Uses
- Herniated disk
- Home Remedies
- House Plants
- Humalog®
- Hydrogen Peroxide
- Hyperglycemia
- Hypoglycemia
- Hyperkalemia
- Hypokalemia
- Hypertension
- Hypotension
- Important Numbers
- Insomnia
- Insulin
- Juice Recipes
- Karma
- Kidney Cysts
- Kidney Disease
- Kinds of Tea
- Lantus®
- Lemon Cleanse
- Logger vs Lineman
- Macaroni!!
- Medicare
- Mental Health
- MO HealthNet
- Moon Phases
- Mounjaro®
- MRI Scan
- My Athletic Shoes
- My Boots & Spurs
- My Cowboy Hats
- Myelography
- Mystical Unicorn
- Nasal Polyps
- Natal Astrology Chart
- Never Forget
- Nuclear Medicine
- Nutrition - Adults
- Nutrition - Adults, Older
- Nutrition - Kids
- Obesity
- One Little Rose
- Orchid Growing
- Orchid Sources
- Pagan Humor
- Pagans vs.Wiccans
- Parking Spaces
- PayPal.Me
- Pentagram vs. Pentacle
- Perennials
- Peripheral Artery Disease
- PET/CT Scan
- PET Scan
- Phobias A-Z
- Plant Care
- Plant Zone Map
- Potassium
- Propagating Plants
- Prurigo Nodularis
- Psychic Gifts
- PVC's
- Quit Smoking
- Recipes I like
- Red Yeast Rice
- Roses
- Runes
- Sadie & Beethoven
- Salt & Sodium
- Salt Water Flush
- Sciatica
- Service Animals
- Shape Shifters
- Sleep Apnea
- Sleep Disorders
- Sleep Studies
- Smile
- SPECT Scan
- Speed Test
- Spices You Need
- Spices I Have
- Spinal Stenosis
- Stents
- Steel Toe vs. Comp. Toe
- Stress Test - Exercise
- Stress Test - Nuclear
- Sugars - Sweeteners
- Superstitions
- Symbols
- Tarot
- The Ten Commandments
- Tools of the Craft
- Top Expensive Movies
- Top Modern Westerns
- Top 100 Westerns
- Toyota Yaris 2008
- Toyota Yaris 2012
- Trazodone
- Tree, Calamondin Orange
- Tree, Lemon (Meyer)
- Tree, Lime
- Tree Signs
- Ultrasound
- US Bill of Rights
- US Constitution
- US Declaration of Independence
- Vaccines by Age
- Vaccines 0-6 yrs
- Vaccines 7-18 yrs
- Vaccines 19 and up
- Ventricular Fibrillation
- Vertigo
- Vital Records
- Vital Signs
- Vitamin B12
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin K
- Vitamins & Minerals
- Water Therapy
- Weight on other Planets
- Wiccan Rede
- X-Rays
- Yin / Yang
- Zodiac Signs
Needed to read PDF's
Hemoglobin
A1C
(HbA1c) Test
Overview
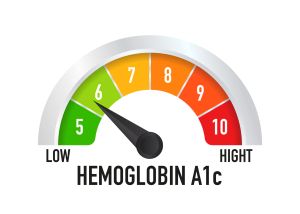
The A1C test is a common blood test for diagnosing diabetes. For people living with diabetes, the test checks how well they manage blood sugar levels. The A1C test also is called the glycated hemoglobin, glycosylated hemoglobin, hemoglobin A1C or HbA1c test.
An A1C test result shows the average blood sugar level over the past 2 to 3 months. The A1C test measures what percentage of hemoglobin in the blood is coated with sugar, also called glycated.
The higher the A1C level is, the poorer the blood sugar management. And the higher the risk of having health concerns related to diabetes.
What is the A1C test?
The A1C test is a blood test that provides information about your average levels of blood glucose, also called blood sugar, over the past 3 months. The A1C test is also the primary test used for diabetes management.
An A1C test may be used to screen for or diagnose:
- Type 2 diabetes. With type 2 diabetes your blood glucose gets too high because your body doesn't make enough insulin to move blood sugar from your bloodstream into your cells, or because your cells stop responding to insulin.
- Prediabetes. Prediabetes means that your blood glucose levels are higher than normal, but not high enough to diagnosed as diabetes. Lifestyle changes, such as healthy eating and exercise, may help delay or prevent prediabetes from becoming type 2 diabetes.
The A1C test is sometimes called the hemoglobin A1C, HbA1c, glycated hemoglobin, or glycohemoglobin test. Hemoglobin is the part of a red blood cell that carries oxygen to the cells. Glucose attaches to or binds with hemoglobin in your blood cells, and the A1C test is based on this attachment of glucose to hemoglobin.
The higher the glucose level in your bloodstream, the more glucose will attach to the hemoglobin. The A1C test measures the amount of hemoglobin with attached glucose and reflects your average blood glucose levels over the past 3 months.
The A1C test result is reported as a percentage. The higher the percentage, the higher your blood glucose levels have been. A normal A1C level is below 5.7 percent.
Why is Hemoglobin A1c important?
What is an A1C test?
An A1C test measures the average amount of glucose (sugar) in your blood over the past three months. The result is reported as a percentage. The higher the percentage, the higher your blood glucose levels have been, on average.
A1C is a simple blood test that healthcare providers use to:
- Diagnose prediabetes. If you have prediabetes, you have a higher risk of getting diabetes and cardiovascular disease.
- Diagnose diabetes. To confirm a diabetes diagnosis, your healthcare professional may look at the results of two blood tests. These can be either two A1C tests or the A1C test plus another test, such as a fasting blood sugar test, also called blood glucose test.
- Check your diabetes treatment plan. The result of a first A1C test also gives you a starting A1C level. It's compared to future A1C test results to see how well your diabetes treatment plan is working.
Healthcare providers do A1C tests in one of two ways:
- A phlebotomist takes a blood sample from your vein and sends it to a lab for analysis (the most common form of the test).
- A provider gets a sample of your blood from a finger prick. They usually get the results from this test within minutes. This form of the test is only for assessing your management, not for diagnosis.
The vein blood test is generally more accurate than the finger prick blood test.
Other names for an A1C test include:
- Hemoglobin A1C.
- HbA1c.
- Glycated hemoglobin.
- Glycohemoglobin test.
What is blood glucose (sugar)?
Glucose (sugar) mainly comes from carbohydrates in the food and drinks you consume. It’s your body’s main source of energy. Your blood carries glucose to all of your body’s cells to use for energy.
Several bodily processes help keep your blood glucose in a healthy range. Insulin, a hormone your pancreas makes, is the most significant contributor to maintaining healthy blood sugar.
If you have consistently elevated blood glucose levels (hyperglycemia) — and an elevated A1C result — it usually indicates diabetes. Diabetes develops when your pancreas doesn’t make any insulin or enough insulin, or your body isn’t using insulin properly.
When would I need an A1C test?
If you have diabetes, you should have an A1C test two or more times a year to see how well your management plan is working. Your healthcare team will recommend exactly how often you should get this test.
If you don’t have a diabetes diagnosis, a healthcare provider may order an A1C test if you have symptoms of the condition, including:
- Intense thirst (polydipsia).
- Increased urination (peeing).
- Blurry vision.
- Fatigue, or feeling tired all the time.
You may also get an A1C test to screen for Type 2 diabetes if you’re at risk for the condition.
Risk factors include:
- Family history of Type 2 diabetes.
- Personal history of gestational diabetes.
- Obesity.
- Lack of activity or exercise.
- Being over the age of 35.
How often do I need an A1C test?
How often you need an A1C test depends on the type of diabetes, your treatment plan, your treatment goals and what your healthcare professional decides. For example, you may have an A1C test:
- Once every year if you have prediabetes.
- Twice a year if you don't use insulin and your blood sugar level stays within your target range.
You may need A1C tests more often if you use insulin or if have trouble keeping your blood sugar level within your target range. You also may have A1C tests if your healthcare professional changes your diabetes treatment plan or you begin taking a new diabetes medicine.
Test Details
How is A1C calculated?
A1C testing relies on hemoglobin. Hemoglobin is the part of the red blood cell that carries oxygen throughout your body. When you have glucose in your blood, it sticks to hemoglobin. This is called glycation. The more glucose is in your blood, the more it sticks. And it can stay there for around three months — about how long the average red blood cell lives.
The A1C test measures the average amount of glucose that’s been attached to hemoglobin over time. Because the A1C test measures glucose levels over a period of time, it provides more information about blood sugar than a single blood sugar test.
Do I need to fast for an A1C test?
No, the test doesn't require fasting beforehand, so you’re free to eat and drink normally. But if you have other blood tests scheduled at the same time, they may require special prep. Check with your doctor.
What should I expect during an A1C test?
During the A1C test, a member of your healthcare team takes a blood sample by putting a needle into a vein in your arm or pricking your finger with a small, pointed tool.
Blood taken from a vein goes to a lab for testing. Your healthcare team may look at blood from a finger prick for results right away. You have this in-office test only to check on your treatment plan. You won't have it for diagnosis or screening.You can expect the following during an A1C test that involves a sample from your vein, or a blood draw:
- You’ll sit in a chair, and a phlebotomist will check your arms for an easily accessible vein. This is usually in the inner part of your arm on the other side of your elbow.
- Once they’ve located a vein, they’ll clean and disinfect the area.
- They’ll then insert a small needle into your vein to take a blood sample. This may feel like a small pinch.
- After they insert the needle, a small amount of blood will collect in a test tube.
- Once they have enough blood to test, they’ll remove the needle and hold a cotton ball or gauze on the site to stop the bleeding.
- Finally, they’ll place a bandage over the site, and you’ll be finished.
You can expect the following during a finger prick A1C test:
- A healthcare provider will ask you which finger you’d like them to use.
- They’ll disinfect your fingertip with an alcohol swab and prick it with a small needle called a lancet, which is usually contained within a small plastic device.
- They’ll squeeze your fingertip to form a drop of blood and collect the drop in a small plastic container.
- After they have enough blood for the test, they’ll give you a cotton ball or gauze to hold against your fingertip to stop the bleeding.
- The results are usually ready within minutes.
What are the risks of an A1C test?
Blood tests are a very common and essential part of medical testing and screening. There’s very little risk to having either type of A1C test. You may have slight tenderness or a bruise at the site of the blood draw or finger prick, but this usually resolves quickly.
Results and Follow-Up
What does my A1C mean?
An A1C test result is reported as a percentage. The number represents the portion of hemoglobin proteins that are glycated, or holding glucose. The higher the percentage, the higher your blood sugar levels have been over the last few months.
For diagnosing purposes, an A1C level of:
- Less than 5.7% means you don’t have diabetes.
- 5.7% to 6.4% signals prediabetes.
- 6.5% or higher usually indicates Type 2 diabetes (or Type 1 diabetes).

If you already have diabetes, an A1C result is a glimpse into how well your management plan has been working over the last three months. Management may involve oral pills, taking insulin, monitoring blood sugar levels and/or lifestyle changes, such as diet and exercise. Your A1C can help you and your provider determine if you should adjust any part of your treatment plan.It’s important to remember that your A1C (if you have diabetes) is just an average measurement of your blood sugar over a few months. It’s not a grade or the ultimate determiner of whether you’re living a healthy life. Know that your A1C will change over your lifetime and that there are steps you can take to improve your diabetes management and A1C level, if needed.
A1C and estimated average glucose (eAG)
Another term you may come across when finding out your A1C is eAG. Your doctor might report your A1C results as eAG. eAG is similar to what you see when monitoring your blood glucose at home on your meter. However, because you are more likely to check your blood glucose in the morning and before meals, your meter readings will likely be lower than your eAG.
Some laboratories report your A1C results as a percentage in addition to the corresponding estimated average glucose (eAG).
The eAG calculation converts the A1C percentage to the same units you use with at-home glucose meters (glucometers) — milligrams per deciliter (mg/dL) or millimoles per liter (mmol/L). Just like your A1C is an average, the eAG is a single number that represents your average blood sugar level over the past three months.
For example, an A1C level of 7% equates to an eAG of 154 mg/dL (8.6 mmol/L). An A1C level of 9% equates to an eAG of 212 mg/dL (11.8 mmol/L).
Comparison of A1C and eAG meter readings
| A1C | eAG | ||
| % | mg/dL | mmol/L | |
| In Range | < 5.7 | < 117 | < 6.5 |
| Prediabetes | 6 | 126 | 7.0 |
| Diabetes | 6.5 | 140 | 7.8 |
| 7 | 154 | 8.6 | |
| 7.5 | 169 | 9.4 | |
| 8 | 183 | 10.0 | |
| 8.5 | 197 | 11.0 | |
| 9 | 212 | 11.8 | |
| 9.5 | 226 | 12.6 | |
| 10 | 240 | 13.4 | |
| 11 | 269 | 14.9 | |
| 12 | 298 | 16.5 | |
| 13 | 326 | 18.1 | |
| 14 | 355 | 19.7 | |
What is a normal A1C?
For people without diabetes, a normal A1C is below 5.7%.
For people with diabetes, what’s “normal” and healthy for you depends on your goals and access to diabetes management medication and tools. Together, you and your healthcare provider will determine an A1C range that should be your target goal. This will likely change throughout your life.
In general, the American Diabetes Association recommends that the goal for most adults with diabetes should be an A1C of 7% or lower.
Your A1C goals may be above 7% if you have:
- Limited life expectancy.
- Severe low blood sugar (hypoglycemia) episodes or are unable to sense these episodes (hypoglycemia unawareness).
- Advanced diabetes complications, such as chronic kidney disease, nerve problems or cardiovascular disease.
On the other hand, healthcare providers typically recommend that people with Type 1 diabetes who are pregnant try to maintain an A1C of 6.5% or lower throughout their pregnancy. This is to try to lower potential health risks for the fetus and to try to prevent fetal macrosomia.
Blood Glucose Measurements Compared with A1C Measurements over 4 Days
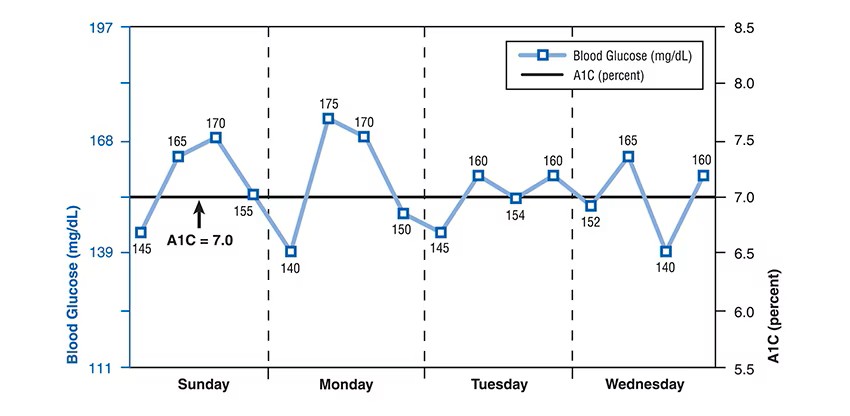
Blood glucose (mg/dL) measurements were taken four times per day (fasting or pre-breakfast, pre-lunch, pre-dinner, and bedtime).
The straight black line shows an A1C measurement of 7.0 percent. The blue line shows an example of how blood glucose test results might look from self-monitoring four times a day over a 4-day period.
A1C levels by age
Age is one of many factors that affect a person’s blood glucose levels. However, while advancing age is associated with increased blood glucose levels, the changes are often small.
Research from 2019 defined age-related A1C percentage levels in healthy populations as:
| Age group | All respondents | Men | Women |
| 20 to 39 years | 4.0 to 6.0 | 4.1 to 6.1 | 4.0 to 5.8 |
|---|---|---|---|
| 40 to 59 years | 4.1 to 6.2 | 4.0 to 6.2 | 4.1 to 6.1 |
| ≥ 60 years | 4.4 to 6.6 | 4.4 to 6.6 | 4.4 to 6.5 |
What is a dangerous level of A1C?
The higher your A1C levels, especially if they’re consistently high over several years, the more likely you’ll develop complications, such as:
- Retinopathy, Vision loss or blindness
- Nephropathy, Kidney failure
- Neuropathy, or nerve damage, which most commonly affects your hands, feet, arms, and legs
- Gastroparesis, or paralysis of the stomach, in which your stomach cannot properly digest food
- Heart disease.
- Stroke.
Studies have shown that people with diabetes may be able to reduce the risk of diabetes complications by consistently keeping their A1C levels below 7%.
It’s important to remember that other factors can contribute to the development of diabetes complications, such as genetics and how long you’ve had diabetes.
Are A1C tests accurate?
When repeated, the A1C test result can be slightly higher or lower than the first measurement. This means, for example, an A1C reported as 6.8 percent on one test could be reported in a range from 6.4 to 7.2 percent on a repeat test from the same blood sample 7.3 In the past, this range was larger but new, stricter quality-control standards mean more precise A1C test results.
Certain factors can affect the accuracy of A1C tests, including:
- Genetics, such as hemoglobin variants.
- Medical conditions.
- Medications and supplements.
- Errors in the collection, transport or processing of the test.
These factors can make your result falsely low or falsely high. Most of the factors are due to differences in the lifespan and health of your red blood cells.
Hemoglobin variants and A1C results
Hemoglobin variants can affect the results of some A1C tests.
The form of hemoglobin in your blood depends on the genes you inherit from your biological parents. There are many different forms. The most common form is hemoglobin A. Other, less common forms of hemoglobin are called hemoglobin variants.
A hemoglobin variant doesn’t increase your risk of developing diabetes, but it can affect A1C results. Labs have different ways to do A1C tests on blood with a hemoglobin variant.
The most common variants include:
- Hemoglobin C trait: Black people, people of West African descent and people from South and Central America, the Caribbean Islands and Europe are most likely to have this trait.
- Hemoglobin D trait: People who live in China, India, Turkey, Brazil and some parts of Europe are most likely to have this trait.
- Hemoglobin E trait: Asian Americans, especially those of Southeast Asian descent, are most likely to have this trait.
- Hemoglobin S trait: Black people and Hispanic Americans are most likely to have this trait.
A blood test can detect hemoglobin variants. Talk to your healthcare provider if you think you might have a hemoglobin variant that could affect your A1C results.
Causes of falsely low A1C results
The following conditions and situations can cause falsely low A1C results, meaning the result is lower than your actual A1C level:
- Alcohol use disorder.
- Blood transfusion.
- Chronic kidney failure.
- Erythropoietin-stimulating agents (ESAs).
- Hemorrhage (bleeding).
- Living at a high altitude.
- Iron supplementation.
- Cirrhosis of the liver.
- Pregnancy.
- Sickle cell anemia.
- Spherocytosis and hemolytic anemia.
Causes of falsely high A1C results
The following conditions and situations can cause falsely high A1C results, meaning the result is higher than your actual A1C level:
- Anemia, such as iron-deficiency anemia, infection-induced anemia or tumor-induced anemia.
- Certain medications, including immunosuppressant medications and protease inhibitors.
- Hypertriglyceridemia. High triglycerides, a type of fat that circulates in your bloodstream
- Organ transplantation.
- Thalassemia, , a blood disorder that keeps your body from producing a normal amount of hemoglobin and red blood cells.
- Vitamin B12 deficiency.
Can you have a high A1C and not have diabetes?
If you have an elevated A1C (above 6.5%) for the first time, it doesn’t always mean that you have diabetes. Other factors, such as certain medications (like steroids) or sickness can temporarily increase your blood sugar levels. Anemia and other conditions can cause a falsely high A1C result, as well. There also could’ve been an error in the collection, transport or processing of the test.
Healthcare providers rely on more than one test to diagnose diabetes. For example, they may order a fasting blood glucose test or another A1C test. In any case, your provider will carefully interpret your results and discuss them with you.
Limitations of the A1C test
The A1c test is a valuable tool for diagnosing and managing diabetes, but it’s not perfect. As detailed above, it’s not always accurate. Another limitation is that it does not tell you how your blood sugar level fluctuates throughout the day, week, or month. Such fluctuations are particularly common in type 1 diabetes. Because the test only gives an average blood sugar level over the previous 3 months, your result could be the same whether your blood sugar fluctuates a lot or stays steady.
Why is that important? Your goal is to keep your blood sugar level in your desired range as much as possible. Your "time in range" numbers provide a better picture of how well you manage your diabetes day to day and week to week. The A1c was not designed to do that. For that, you need a continuous glucose monitor, which tracks your glucose level 24/7.Some factors may make A1C test results less exact.
These include:
- Pregnancy.
- Recent or heavy blood loss.
- Recently receiving blood from a donor, called a transfusion.
- Sometimes, a condition that results in not having enough red blood cells, called anemia.
- Certain blood conditions, such as sickle cell anemia.
- Other forms of hemoglobin in the body.
Hemoglobin is a protein that carries oxygen through the blood. The most common form of hemoglobin protein is called hemoglobin A. If there are other forms of hemoglobin in the blood, called variants, the A1C test results may not be right. Hemoglobin variants are more common among people of African, Mediterranean or Southeast Asian descent.
If you have a hemoglobin variant, your test may need to go to a special lab. Or you may need another test to diagnose diabetes and check on its treatment.
What A1C goal should I have?
People will have different A1C targets, depending on their diabetes history and their general health. You should discuss your A1C target with your health care professional. Studies have shown that some people with diabetes can reduce the risk of diabetes complications by keeping A1C levels below 7 percent.
Managing blood glucose early in the course of diabetes may provide benefits for many years to come. However, an A1C level that is safe for one person may not be safe for another. For example, keeping an A1C level below 7 percent may not be safe if it leads to problems with hypoglycemia, also called low blood glucose.
Less strict blood glucose control, or an A1C between 7 and 8 percent—or even higher in some circumstances—may be appropriate in people who have
- limited life expectancy
- long-standing diabetes and trouble reaching a lower goal
- severe hypoglycemia or inability to sense hypoglycemia (also called hypoglycemia unawareness)
- advanced diabetes complications such as chronic kidney disease, nerve problems, or cardiovascular disease
This chart details goals for specific groups of people with diabetes, based on age:
| Age | Before meals (fasting) | After eating |
| Children and teens | 90 to 130 mg/dL | |
| Adults | 80 to 130 mg/dL |
< 180 mg/dL (1 or 2 hours after) |
| Pregnant | 70 to 95 mg/dL |
110 to 140 mg/dL (1 hour after); 100 to 120 mg/dL (2 hours after) |
| 65 and older | 80 to 130 mg/dL | |
| Without diabetes | 99 mg/dL or below | 140 mg/dL |
It’s important to remember that age alone isn’t a deciding factor on your blood sugar targets.
When to contact a doctor
A person should make an appointment with their doctor if they:
- have questions or concerns about their treatment plan
- are finding it hard to keep their blood glucose levels within the target range
- have had symptoms of high or low blood glucose levels
- think they might have complications of diabetes
Symptoms of high blood glucose levels include:
- fatigue
- unusual thirst
- frequent urination
- blurred vision
Symptoms of low blood glucose levels include:
- nervousness, irritability, or anxiety
- confusion
- dizziness
- hunger
- shaking
- sweating
Anyone who develops any of the symptoms above or notices other changes in their health should inform a doctor.
Additional Details
Is A1C an accurate representation of diabetes management?
For decades, healthcare providers and people with diabetes have relied on A1C as the main way to gauge how well their management of the condition is working.
For people with Type 1 diabetes, in particular, blood sugar can fluctuate significantly throughout the days, weeks and months. Because of this, A1C isn’t always an accurate measurement of management since it’s based on an average.
For example, a person who has frequent blood sugar fluctuations between significantly low and high episodes may have an A1C of 7%. A person who has blood sugar levels that stay more consistently around 154 mg/dL may also have an A1C of 7%.
More recently, with the invention of continuous glucose monitoring (CGM) devices, providers and people with diabetes have found time in range (TIR) to be a more helpful and accurate representation of diabetes management.
Time in range is the amount of time your blood sugar levels are in a recommended target range. TIR is measured as a percentage. Blood sugar range goals can vary for each person, but a typical target range is between 70 and 180 mg/dL. For most adults with Type 1 diabetes or Type 2 diabetes, providers recommend aiming to have a TIR above 70% (about 17 hours of a 24-hour day).
With CGMs and TIR, providers and people with diabetes can see how often they’re experiencing high or low blood sugar episodes. This can help them more accurately adjust treatment strategies.
Hemoglobin A1c FAQs
What does a hemoglobin A1c test measure?
This test measures your average blood sugar (aka blood glucose) level over the previous 3 months. It is used to diagnose and manage diabetes.
What is a normal A1c range by age?
A1c tests calculate the percentage of blood sugar in your bloodstream. The normal range, meaning you don’t have diabetes, is below 5.7%. That normal range remains the same no matter your age.
Does a high A1c level mean I have diabetes?
Maybe. If you have no symptoms of diabetes when you take the test, your doctor will schedule a follow-up A1c test to confirm the result. Also, several health conditions and other factors can make the A1c test less accurate, potentially causing falsely high or falsely low results. Your doctor should consider these factors when evaluating your A1c test result.
What happens if your hemoglobin is low?
Low levels of hemoglobin keep your body from delivering enough oxygen to tissues. As a result, you feel tired and weak, and your body can’t function like it should.
What happens if your hemoglobin is high?
High levels of hemoglobin thicken your blood. This keeps it from flowing as easily, which means your organs can’t get the amount of oxygen they need. You may get headaches, dizziness, blurred or double vision, itching, and blood clots.
Is high or low hemoglobin bad?
Your hemoglobin levels give your doctor important information about the health of your red blood cells. Both high and low levels of hemoglobin can be signs that your tissues and organs aren’t getting the oxygen they need. They can also indicate underlying problems.
Is high hemoglobin something to worry about?
Some causes of high hemoglobin can be serious, such as bone marrow disease, congenital heart disease, heart failure, and scarred lungs. But other factors that can cause it include time spent at a high altitude and dehydration. Your doctor can test you for conditions that may be raising your hemoglobin levels.
What causes hemoglobin to be a little high?
Most often, high hemoglobin happens because your blood oxygen levels have been low for some time. This might be because of an illness or injury. Your doctor will examine you and may do tests to find out what’s behind your high hemoglobin levels.
One Final Note..
A doctor orders an A1C test to check whether someone has prediabetes or type 1 or 2 diabetes. Doctors also use this test to monitor blood glucose levels in people with diabetes to check how well their treatment plan is working.
A1C test results are usually a percentage but may come as an eAG measurement. Target A1C levels vary from person to person, depending on age, overall health, and other factors.
Having high A1C levels may indicate a person has diabetes or a high risk of related complications. In this case, a doctor will work with the individual to adjust the treatment approach.It can be stressful to see an abnormal or higher-than-you-expected A1C result. Know that having an elevated A1C for the first time doesn’t necessarily mean you have diabetes. Several factors can cause inaccurate results. Your healthcare provider will let you know if you need to undergo further tests. Don’t be afraid to ask your provider questions. They’re available to help you.
If you have diabetes, it’s important to remember that your A1C is just a temporary average of your blood sugar levels. Know that there are steps you can take to change your A1C level. If you’re feeling overwhelmed with diabetes management, talk to your healthcare provider. Together, you can formulate a plan to get closer to your management and A1C goals.
Find me on Social Media
 |
Don't forget to bookmark me to see updates.. Copyright © 2000 - 2025 K.
Kerr |







