- Main Page
- A1C Test
- Advance Directives
- Anxiety
- Aortic Aneurysm
- Aphrodisiacs
- Apple Cider Vinegar
- Arrhythmia
- Atrial Fibrillation - AFib
- Back Pain
- Blood Tests
- Blood Test Tubes
- Blood Types
- BMI Calculator
- Body Mass Index - BMI
- Bone Scan
- BPPV
- Bronchitis
- Cancer - Lung
- Carbohydrates
- Cardiac Catheterization
- Cardiovascular Disease
- Caregiver Glossary
- Caregiver Resources - LGBTQ+
- Caregiver Resources - MO
- Caregiver Resources - USA
- Continuous Glucose Monitors
- Cholesterol
- Citalopram
- COPD
- Coronary Artery Disease
- Cough
- CPAP
- CT scan
- Cyclobenzaprine
- Degenerative Disc Disease
- Depression
- Diabetes Information
- Diabetes - Type 1
- Diabetes - Type 2
- Diabetes - Type 3c
- Diabetes Facts
- Diabetes Care
- Diabetes Care Team
- Diabetes & Fruits
- Diabetes - Gestational
- Diabetes - Pre
- Diabetic Terms
- Diabetes & Vegetables
- Diet - Boiled Egg
- Diet - DASH
- Diet - Fat Burning
- Diet - Mediterranean
- Diet - Military
- Disability
- Disability Permits
- Do Not Resuscitate
- Dupixent®
- Echocardiogram
- E-Cigarettes
- Electrocardiogram
- Electromyography
- Emphysema
- Epidural - Lumbar
- Epidural - Transforaminal
- Epsom Salt
- Facet Arthropathy
- Farxiga®
- Flu - Influenza
- Fluoroscopy
- Gabapentin
- GERD
- Glycemic Index
- Gout
- Headaches
- Healing & Energy Work
- Health Facts
- Health Info. Lines
- Heart Attack
- Heart Disease - Other
- Heart Failure
- Heart Imaging Tests
- Herbal Terms
- Herbal Medicine
- Herb & Oils Uses
- Herniated disk
- HIPAA
- Home Remedies
- Humalog®
- Hydrogen Peroxide
- Hyperglycemia
- Hyperkalemia
- Hyperlipidemia
- Hypertension
- Hypoglycemia
- Hypokalemia
- Hypotension
- Important Numbers
- Indomethacin
- Informed Consent
- Inhalers
- Insomnia
- Insulin
- Juice Fasting
- Juice Recipes
- Kidney Cysts
- Kidney Disease
- Lantus®
- Lemon Benefits
- Lime Benefits
- Liver Disease
- Lumbar Retrolisthesis
- Medicaid
- Medical Specialties
- Medicare
- Medicare - Your Rights
- Melatonin
- Men's Health
- Mental Health
- MO HealthNet
- Mounjaro®
- MRI Scan
- Myelography
- Naproxen
- Nasal Polyps
- Nuclear Medicine
- Nutrition - Adults
- Nutrition - Adults, Older
- Nutrition - Kids
- Obesity
- Otolaryngologist
- Oxycodone-Acetaminophen
- Pain Management
- Peripheral Artery Disease
- Parking Spaces
- PET/CT Scan
- PET Scan
- Potassium
- Prescription Drugs
- Prurigo Nodularis
- PVC's
- Quetiapine
- Quit Smoking
- Radiculopathy
- Red Yeast Rice
- Reiki
- Salt & Sodium
- Salt Water Flush
- Sciatica
- Service Animals
- Sleep Apnea
- Sleep Disorders
- Sleep Studies
- SPECT Scan
- Spinal Stenosis
- Statins
- Stents
- Stress Test - Exercise
- Stress Test - Nuclear
- Sugars - Sweeteners
- Support Groups
- Tardive Dyskinesia
- Testosterone
- Trazodone
- Ultrasound
- Vaccines 19 and up
- Vaccines by Age
- Vaccines 0-6 yrs
- Vaccines 7-18 yrs
- Ventricular Fibrillation
- Vertigo
- Vital Records
- Vital Signs
- Vitamin B12
- Vitamin C
- Vitamin D
- Vitamin E
- Vitamin F
- Vitamin K
- Vitamins and Minerals
- Vitamins Recommended
- Water Benefits
- X-Rays
Needed to read PDF's
Spinal Stenosis
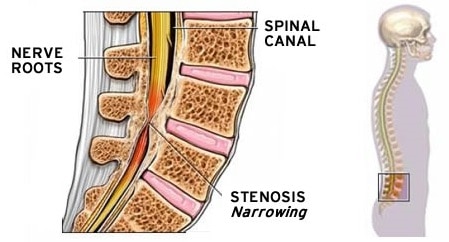
What is Spinal Stenosis?
There are many different structures in the anatomy of the back that work together to support your body.
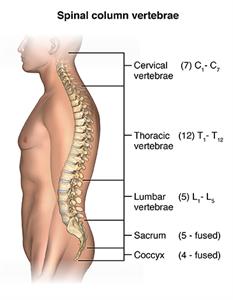
There are four regions of the spine:
- Cervical spine.
- Thoracic spine.
- Lumbar spine.
- Sacrum and coccyx.
Spinal stenosis is a condition where the spinal canal narrows. This can put pressure on the nerves in the spine. Symptoms include back pain, numbness, tingling, and weakness in the legs or arms.
There are two main types of spinal stenosis. Cervical stenosis affects the neck, while lumbar stenosis impacts the lower back. Factors like degenerative disc disease, herniated discs, and osteoarthritis can cause it.
Symptoms of spinal stenosis can vary from mild to severe. They may get worse over time if not treated. Luckily, there are treatments to help manage symptoms and improve life quality for those with this condition.
What is Spinal Stenosis?
Spinal stenosis is when the spinal canal gets smaller. This canal is inside the spine and holds the spinal cord and nerves. When it narrows, it can press on these nerves, causing symptoms.
This narrowing is called spinal canal narrowing. It can lead to nerve compression, where nerves get squeezed. This can cause pain, numbness, tingling, and weakness in different parts of the body.
In severe cases, spinal cord pressure can happen. This can lead to more serious symptoms and problems.
Spinal stenosis can happen in different parts of the spine:
- Cervical spine (neck): Common Condition
- Thoracic spine (mid-back): Rare Condition
- Lumbar spine (lower back): Common Condition
The most common places affected are the neck and lower back. Cervical stenosis can cause neck, shoulder, arm, and hand symptoms. Lumbar stenosis affects the lower back, buttocks, legs, and feet.
Knowing where and how much the spinal canal narrows is key for a correct diagnosis and treatment.
Causes of Spinal Stenosis
Several factors can lead to spinal stenosis, a condition where the spinal canal narrows. Common causes include degenerative disc disease, herniated or bulging discs, and osteoarthritis.
Degenerative Disc Disease
Degenerative disc disease is a natural aging process. The discs between vertebrae start to deteriorate. As they lose hydration and elasticity, they thin out, reducing space between vertebrae.
This narrowing can put pressure on the spinal cord and nerves. It leads to symptoms of spinal stenosis.
Herniated or Bulging Discs
Herniated discs, or bulging discs, happen when the soft inner material of a disc bulges out. This can press on the spinal cord or nerves, causing pain, numbness, and weakness.
They can be caused by age, injury, or too much strain on the spine.
Osteoarthritis and Bone Spurs
Osteoarthritis is a degenerative joint disease that affects the spine. It causes the cartilage between vertebrae to break down. As cartilage wears away, bones rub against each other, forming bone spurs.
These bony projections can narrow the spinal canal. They can compress the spinal cord or nerves, causing spinal stenosis.
The following table summarizes the main causes of spinal stenosis:
| Cause | Description | Effect on Spinal Canal |
| Degenerative Disc Disease | Discs lose hydration and elasticity, becoming thinner | Narrowing of space between vertebrae |
| Herniated or Bulging Discs | Soft inner material protrudes through a tear in the outer layer | Compression of spinal cord or nerves |
| Osteoarthritis and Bone Spurs | Cartilage breaks down, leading to bone spur formation | Narrowing of spinal canal |
It’s important to note that while these conditions are common causes of spinal stenosis, not everyone with degenerative disc disease, herniated discs, or osteoarthritis will develop spinal stenosis. Genetics, lifestyle, and overall health also play a role in developing this condition.
Other Conditions
The following conditions also may cause spinal stenosis:
- Tumors of the spine are abnormal growths of soft tissue that may affect the spinal canal directly by causing inflammation or growth of tissue into the spinal canal. This can narrow the space and cause bone changes, leading to spinal stenosis. Some people develop a rare disorder called epidural lipomatosis, which happens when fat builds up on or around the lining of the spine.
- Fractures due to trauma (injury) or other medical conditions may cause misalignment of the spine and the spinal canal or cause fractures that produce fragments of bone that penetrate the canal.
- Paget's disease of bone is a chronic (long-lasting) disorder that causes bones to grow larger and become weaker than normal. As Paget’s disease progresses, new bone forms at a faster rate than the rate at which old bone is removed. However, the new bone does not form correctly, leading to larger bones that are misshapen, weaker, and softer than normal bone. This can cause problems with blood supply and bone structure, which changes the spaces in the spinal canal, leading to spinal stenosis.
- Ossification of the posterior longitudinal ligament happens when calcium deposits form on the ligament that runs up and down behind the spine and inside the spinal canal. These deposits turn the fibrous tissue of the ligament into bone and may press on the nerves in the spinal canal.
Inherited Conditions
Some people are born with a condition that can cause spinal stenosis. These conditions cause the spinal canal to narrow, leading to spinal stenosis. For example:
- Congenital stenosis happens when you are born with a small and narrow spinal canal.
- Scoliosis is a curvature of the spine.
- Achondroplasia is an inherited condition that causes problems with bone formation in the spine and other bones in the body.
Types of Spinal Stenosis
Spinal stenosis can happen in different parts of the spine. This leads to different symptoms and challenges. The two main types are cervical stenosis and lumbar stenosis. Each affects a specific area and causes unique discomfort.
Cervical Stenosis
Cervical stenosis happens in the neck area of the spine. When the spinal canal narrows here, it can press on the spinal cord and nerve roots. This can cause various symptoms.
People with cervical stenosis often feel neck pain and stiffness. They may also have numbness or weakness in their arms, hands, or fingers. In severe cases, they might have trouble balancing and coordinating.
Lumbar Stenosis
Lumbar stenosis occurs in the lower back area of the spine. When the spinal canal narrows here, it can compress nerves. This affects the nerves in the lower back and legs.
The most common symptom is lower back pain. This pain may be accompanied by numbness, weakness, or cramping in the legs and feet. These symptoms often get worse when walking or standing. They may feel better when sitting or bending forward.
It’s important to understand the differences between cervical and lumbar stenosis. Both involve narrowing of the spinal canal. But they affect different areas of the body. They need different treatments to manage symptoms and improve quality of life.
Symptoms of Spinal Stenosis
Spinal stenosis can cause a variety of symptoms. These depend on where and how much the spinal canal narrows. Common symptoms include back pain, leg pain, numbness, weakness, and sciatica. These symptoms often get worse when standing or walking for a long time. They can feel better when sitting or bending forward.
Many people with spinal stenosis complain of back pain. This pain might stay in one spot or spread to the legs, known as sciatica. Sciatica happens when nerves in the spine get compressed. This leads to pain, numbness, and weakness in the legs.
The symptoms can differ based on the type of spinal stenosis:
| Type of Spinal Stenosis | Symptoms |
| Cervical Stenosis |
|
| Lumbar Stenosis |
|
If you have ongoing back pain, leg pain, numbness, weakness, or sciatica, see a doctor. Early diagnosis and treatment can help manage symptoms. This can also prevent the condition from getting worse.
Diagnosing Spinal Stenosis
Getting a correct spinal stenosis diagnosis is key to finding the right treatment. Doctors use a detailed physical exam and advanced imaging to spot spinal canal narrowing. This helps them understand how severe it is.
Physical Examination
Your doctor will check your strength, feeling, reflexes, and how well you move during a physical exam. They might ask you to do certain movements to see if they cause pain. This helps them pinpoint where and how bad your symptoms are.
During your appointment with your healthcare provider, they will inquire about your specific symptoms, including their severity and duration.
A physical exam that focuses on your neck, back, and extremities will also be performed. Specifically, your healthcare provider will check your reflexes, assess for muscle weakness and sensory disturbances, and check your gait, balance, and pain level.
Imaging Tests
To confirm spinal stenosis, your doctor might suggest one or more imaging tests:
| Imaging Test | Description |
| X-rays | X-rays show the bones in your spine clearly. They can spot changes in vertebrae or a narrowed spinal canal. An X-ray of the spine can be useful for identifying the culprit behind a person's spinal stenosis, such as a spinal tumor, traumatic injury, spinal arthritis, or an inherited abnormality. |
| MRI | Magnetic Resonance Imaging (MRI) gives detailed views of soft tissues, nerves, and discs. It helps find compression or damage. An MRI of the spine is the best test for diagnosing spinal stenosis. It can reveal the precise location of the stenosis and help pinpoint exactly what is placing pressure on the spinal cord and nerve roots. |
| CT Scan | Computerized Tomography (CT) scans use X-rays from different angles. They create detailed images of your spine’s bony structures and any narrowing. A CT scan is more sophisticated than an X-ray and can reveal areas of compression within the spinal canal, as well as bony growths from osteoarthritis (called bone spurs) and fractures. |
| Myelogram | A myelogram is like a CT scan, but entails injecting dye into the cerebrospinal fluid surrounding the spinal cord and nerves. This test may be used in people who cannot undergo an MRI (e.g., patients with cardiac pacemakers). |
Your doctor will look at your physical exam and imaging test results. They’ll then create a treatment plan tailored to you. This plan aims to ease your symptoms and enhance your life quality.
Non-Surgical Treatments for Spinal Stenosis
Many people with spinal stenosis find relief without surgery. These non-surgical methods aim to ease pain, boost mobility, and stop the condition from getting worse. The main treatments are physical therapy, pain meds, and epidural steroid shots.
Physical Therapy and Exercise
Physical therapy is key for spinal stenosis. A physical therapist creates a plan to keep you flexible, strong, and upright. Exercises might include stretching, strengthening, and low-impact cardio.
| Exercise Type | Benefits |
| Stretching | Improves flexibility and reduces muscle tension |
| Core strengthening | Supports the spine and improves posture |
| Low-impact aerobic exercise | Promotes circulation and overall fitness |
Doing exercises at home is also important. It helps keep up with progress and manage symptoms over time.
Pain Medication and Anti-inflammatories
Pain meds can help with spinal stenosis pain. Over-the-counter and prescription drugs like NSAIDs can cut down on inflammation and pain. For severe cases, stronger meds might be needed. Always follow your doctor’s advice on using these drugs.
Epidural Steroid Injections
Epidural steroid shots target the spine’s affected area. They offer temporary relief from pain and swelling. This lets patients do more in physical therapy and exercise. The effects can last months, and you can get up to three shots a year.
Even though non-surgical treatments work well for many, some might need surgery if these methods don’t help enough. Working with a healthcare team and trying non-surgical options first can help manage the condition and keep a good quality of life.
Complementary Therapies
While the scientific evidence backing up their benefit is scant, one or more complementary therapies (used under the guidance of your healthcare provider) may be incorporated into your treatment plan to help soothe pain from spinal stenosis.
Some of these therapies may include:
- Massage therapy
- Acupuncture
- Chiropractic care
Surgical Options for Spinal Stenosis
When non-surgical treatments don’t work, surgery might be needed. The aim of spinal stenosis surgery is to make more space in the spinal canal. This helps relieve pressure on the spinal cord and nerves. The surgery type depends on where and how severe the stenosis is.
Surgeries to create more space within the spinal canal may include:
- Laminectomy: This surgery removes the back part of the affected spinal bone. This part of the bone is called the lamina. This process eases pressure on the nerves by making more space around them. Sometimes, that bone may need to be linked to nearby spinal bones with metal hardware and a bone graft.
- Laminotomy: This surgery removes only part of the lamina. The surgeon carves a hole just big enough to relieve pressure in a specific spot.
- Laminoplasty: This surgery is done only on spinal bones in the neck. It makes the space within the spinal canal bigger by creating a hinge on the lamina. Metal hardware bridges the gap in the opened section of the spine.
- Foraminotomy: The foramen is the area in your vertebrae where the nerve roots exit. This procedure involves removing bone or tissue in this area to provide more space for the nerve roots.
- Spinal fusion: Healthcare providers use spinal fusion as a last option. They only consider it if you have radiating nerve pain from spinal stenosis, your spine is not stable and other treatments haven’t helped. Spinal fusion surgery permanently joins (fuses) two vertebrae together.
Minimally invasive surgery is also used for spinal stenosis. These surgeries have smaller incisions and less tissue disruption. This can lead to quicker recovery times. Some examples include:
| Procedure | Description |
| Microendoscopic decompression | Uses a small camera and specialized instruments to remove bone and ligament through a tiny incision |
| Interspinous process spacers | Implants a device between the spinous processes to maintain space in the spinal canal |
| Coflex interlaminar stabilization | Places a U-shaped implant between two vertebrae to provide stability and maintain the decompression |
Surgical risks. There are minor risks associated with every surgical procedure. These include bleeding, infection, blood clots, and reaction to anesthesia. These risks are usually very low.
Elderly people, overweight people, diabetics, smokers, and those with multiple medical problems have higher rates of complications from surgery.
Specific complications from surgery for spinal stenosis include:
- Tear of the sac covering the nerves (dural tear)
- Failure of the bone fusion to heal if a fusion is performed
- Failure of screws or rods if a fusion is performed
- Nerve injury
- Need for further surgery
- Failure to relieve symptoms
- Return of symptoms
Surgical outcomes. Overall, the results of laminectomy with or without spinal fusion for lumbar stenosis are good to excellent in the majority of patients. Patients tend to see more improvement of leg pain than back pain, and most people can resume a normal lifestyle after a period of recovery from surgery.
Recovery time after surgery varies based on the procedure and the patient’s health. Physical therapy is often needed to help regain strength and mobility. While surgery can offer relief, it’s key to talk about risks and benefits with a spine surgeon before making a decision.
Lifestyle Changes to Manage Spinal Stenosis
Medical treatments help with spinal stenosis symptoms. But, lifestyle changes are key to managing it better. Healthy habits and daily activity changes can reduce pain and keep you moving.
Maintaining a Healthy Weight
Being overweight strains the spine, making spinal stenosis worse. Eating right and exercising can ease this pressure. Even a little weight loss can help a lot.
Staying Active and Exercising Regularly
Exercise keeps you flexible and strong. Try walking, swimming, or using an elliptical. These activities boost heart health and strengthen spine-supporting muscles. Stretching also helps keep muscles loose and prevents spasms.
Always talk to a doctor or physical therapist before starting any exercise. They’ll help create a plan that fits your needs.
Practicing Good Posture
Good posture lessens spine pressure and eases symptoms. Sit straight with feet on the floor. Stand with shoulders back, head up, and weight balanced.
Using ergonomic furniture and lifting correctly also helps. These habits protect your spine and prevent injuries.
By making these lifestyle changes, you can manage spinal stenosis better. These habits won’t replace medical treatment but can enhance your life quality.
Complications and Long-Term Outlook
Spinal stenosis can lead to serious complications if not treated properly. Chronic pain is a common issue, affecting a person’s daily life. The constant pressure on nerves can make simple tasks hard to do.
In severe cases, spinal stenosis can cause disability. This can lead to weakness, numbness, and loss of function in limbs. It may require the use of assistive devices or ongoing care.
The outlook for spinal stenosis depends on several factors. These include the condition’s severity, its cause, and the treatment’s success. Early diagnosis and proper management are key to avoiding complications. By following a healthy lifestyle and staying active, many can manage their symptoms well.
FAQ's
Q: What is the difference between cervical and lumbar stenosis?
A: Cervical stenosis happens in the neck. It can cause pain, numbness, or weakness in the neck, shoulders, arms, and hands. Lumbar stenosis is in the lower back. It can cause pain, numbness, or weakness in the lower back, buttocks, legs, and feet, and even sciatica.
Q: Can spinal stenosis be cured?
A: There’s no cure for spinal stenosis. But, there are treatments to manage symptoms and improve life quality. Non-surgical options include physical therapy, exercise, pain meds, and epidural injections. Surgery might be needed for severe cases to relieve pressure.
Q: Is spinal stenosis a serious condition?
A: Yes, spinal stenosis can be serious if not treated. It can lead to chronic pain, disability, and complications. In severe cases, it may cause permanent nerve damage or paralysis. Early treatment is key to managing symptoms and preventing further damage.
Q: Can lifestyle changes help manage spinal stenosis?
A: Yes, lifestyle changes can help manage symptoms. Keeping a healthy weight, staying active, exercising regularly, and good posture can reduce pain and improve flexibility. It’s important to work with a healthcare provider to create a personalized treatment plan.
Q: How is spinal stenosis diagnosed?
A: Diagnosis involves a physical exam and imaging tests. The physical exam checks symptoms, range of motion, and neurological function. Imaging tests like X-rays, MRI, and CT scans show detailed spine images, helping identify spinal stenosis.
Q: What are the risk factors for developing spinal stenosis?
A: Risk factors include age over 50, spinal injuries or surgeries, congenital deformities, and certain medical conditions like osteoarthritis and rheumatoid arthritis.
Q: What is the long-term outlook for people with spinal stenosis?
A: The outlook varies based on the condition’s severity and treatment success. Many manage symptoms well and live active lives. But, in some cases, it may worsen, leading to chronic pain or disability. Regular check-ups with a healthcare provider are vital to monitor symptoms and adjust treatment.
One Final Note..
Back and neck pain can interrupt your daily life. The good news is that there are many treatment options for spinal stenosis. See your healthcare provider to discuss your options. They’re available to help.
You cannot stop spinal stenosis from progressing. However, with the right treatment plan—one that includes a combination of regular exercise and medication—you can optimize your pain control and mobility and live well.
If you or a loved one is suffering from spinal stenosis, it's a good idea to obtain a consultation from someone who specializes in back disorders, such as a rheumatologist or physiatrist, so you can get guidance from an expert on your condition.
Find me on Social Media
 |
Don't forget to bookmark me to see updates.. Copyright © 2000 - 2025 - K. Kerr Most recent revision January 22, 2026 12:20:32 PM
|











